Descriptive analysis of prevalence and medical expenses of cancer, cardio-cerebrovascular disease, psychiatric disease, and musculoskeletal disease in Korean firefighters
Article information
Abstract
Background
Firefighters are exposed to many dangerous working conditions. Many studies have identified the risk of disease for firefighters, but only a few studies have addressed the medical expenses of firefighters, which represents a concrete scale of disease. Our purpose in this study was to determine the medical expenditures of firefighters to assess the overall scale of disease in Korea. We focused on cancer, mental disorders, cardio-cerebrovascular disease, and musculoskeletal disease, the prevalence of which was expected to be high in firefighters.
Methods
This study utilized National Health Insurance Service data. We targeted firefighters, police officers, and government officials. We classified disease based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems codes. We compared prevalence by the age-standardized prevalence rate, considering standard distribution of the population. Medical expenditure of disease was defined as outpatient fees, hospitalization fees, and drug costs. Total medical expenditures were calculated by the sum of those 3 categories.
Results
The age-standardized prevalence of cancer, mental disorders, and cardiovascular disease in firefighters was slightly higher than or similar to that of government officials and police officers (no significant difference). However, medical expenditures for stomach cancer, mental disorders, and most cardio-cerebrovascular diseases were higher in firefighters than in others. In particular, firefighters spent 12 times more money for ischemic heart disease than did government officials. Of musculoskeletal diseases, lumbar disc disorder had the highest expenditures among firefighters.
Conclusions
The age-standardized prevalence of most of diseases of firefighters was not as high as in the other groups, but the medical expenses of firefighters were much higher than those of government officials and police officers.
BACKGROUND
Firefighters are well-known public safety professionals [1]. It is well known that the health of firefighters is often endangered [2]. The mortality and accident rates of firefighters are higher than the industrial accident rates of general workers. From 2000 to 2008, the average mortality rate per 10,000 firefighters was 28.94, which was about 1.8 times higher than the 15.5 per 10,000 industrial accidents in 2010 [3].
The responsibilities of a firefighter are defined by law as fire suppression, support for fire suppression, emergency medical services (EMS; 119 paramedics), and other activities to establish or maintain safety; for example, removal of objects that may fall, capture or eradication of harmful animals, and supply of light during a blackout [1]. In the course of their jobs, firefighters are exposed to many carcinogens, including arsenic, asbestos, benzene, 1,3-butadiene, cadmium, formaldehyde, sulfuric acid, and also radioactivity and radionuclides [4]. The morbidity of specific cancer types, e.g., colorectal cancer, urologic cancers, and non-Hodgkin's lymphoma, in Korean firefighters is higher than in the general population [5]. Also, most firefighters are shift workers who are subject to an on-call system. Shift work causes mental stress as well as sleep disorders and even certain specific cancer types, like breast cancer, prostate cancer, and colorectal cancer [6]. For these reasons, the International Agency for Research on Cancer has classified firefighters as having a group 2B carcinogen job exposure [4].
The risk of cerebrovascular disease in firefighters is also higher than in the general population [7]. Compared to office workers, firefighters have higher metabolic demands for firefighting tasks [8]; because of this high physical burden, cerebrovascular disease events can occur when firefighters are in emergency situations, doing strenuous work [9]. In a 2017 cohort study [7], firefighters had a higher risk for angina pectoris (hazard ratio [HR]: 1.06; 95% confidence interval [CI]: 1.02–1.10) and myocardial infarction (HR: 1.21; CI: 1.10–1.32) than did government officials.
Because of high job stress, challenging physical environments, insufficient job control, and frequent interpersonal conflicts, even violence, the prevalence of musculoskeletal disease in firefighters is also higher than in the general population [10]. Especially, the activities of rescue and EMS causes high muscle fatigue with continuous work [11]. Even more telling, the incidence of post-traumatic stress disorder (PTSD) in firefighters is higher than in the general population, because they often deal first-hand with casualties and witness horrendous accidents [12]. For firefighters, the hazard of PTSD is higher than for government officials (HR: 1.40; CI: 1.26–1.56) [7].
Police officers are also public safety professionals and are also exposed to similar hazardous job conditions [13]. They often experience high metabolic demands, must respond to traumatic events, and have a shiftwork schedule [14]. To protect people from criminals, police are often dispatched to fire scenes [13]. Because of these similarities in job conditions, many studies evaluate health of firefighters in comparison with that of police officers [7]. Here, we also compare illness prevalence and medical expenses of such public service providers to those of government officials, representative of white-collar workers. Government officials were used as a control group not exposed to either chemical carcinogens or shiftwork [7].
Medical expenses can be used as an epidemiological indicator which reflects the overall scale of a specific disease, even if it was developed as an economic indicator. There have been many attempts to elucidate the burden of disease by calculating medical expenses [15]. For example, the economic burdens of cerebrovascular disease, ischemic heart disease, and cancer are much higher than of other diseases [16], partly because it is hard to go back to the workplace with any of these conditions [17]. Economic burden includes not only direct medical expenditures but also costs derived from the disease, such as job loss and care costs [18]. Also, to be considered are the medical expenditures of chronic diseases such as diabetes, hypertension, and cancer, which induce continuous medical expenditures [19]. Comparing prevalence and medical costs is important to determine the exact scale of medical expenditures for the establishment of health-promoting policies and disease prevention measures [20].
METHODS
Data collection
This study used National Health Insurance Service (NHIS) data, which includes claim data of the entire Korean population. NHIS is the national health insurance system operated by a single insurer for the whole country. Every insured person is given a unique identification code called a resident registration number, through which every health insurance claim is recorded. Every utilization of the health care system is recorded, including number and visit dates of outpatients, costs of hospitalization, drug costs, region, and type of health care system.
Our research objective was to compare the prevalence rates and medical expenditures of firefighters and 2 other occupational groups, police officers (a similar occupational group) and government officials (representative of white-collar workers). Government officials were used as a control group not exposed to chemical carcinogens or shiftwork. Our analysis data set was created by linking the NHIS qualification database with the NHIS medical care database. To extract the occupations, we targeted the public servants category of NHIS insurance coverage. A “firefighter” was defined as a person whose workplace was a fire station for 2 consecutive years in 2010 and 2011, and a “police officer” was defined as a person whose workplace was a police station for the same study period. Among police officers, people were excluded whose workplaces were the Ministry of Land, Infrastructure and Transport Department, the Korea Coast Guard, the Central Police Academy, the Police Human Resources Development Institute, the Korean National Police University, the National Police Hospital, and Special Judicial Police Officers. “Government officials” were all other public servants, excluding teachers.
Using the customized database of the NHIS, we first selected diseases that could be easily be prevented by systematic intervention. Considering impacts of such intervention, we also selected diseases with a relatively high prevalence in firefighters in 2017. These diseases comprised cancer, mental and behavioral disorders, cardio-cerebrovascular disease, and musculoskeletal disease. Management of workplace air contaminant exposure decreases risk of cancer, and early intervention and prevention of musculoskeletal and cardio-cerebrovascular disease are cost-effective [21].
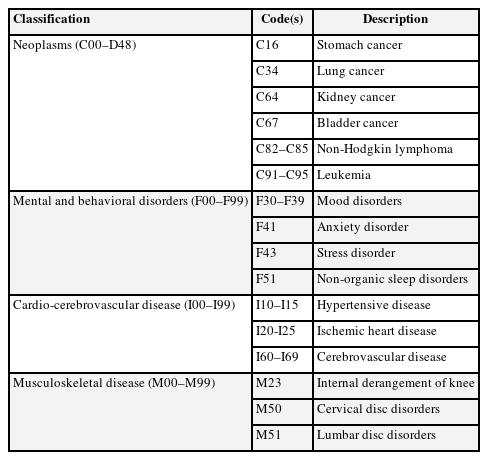
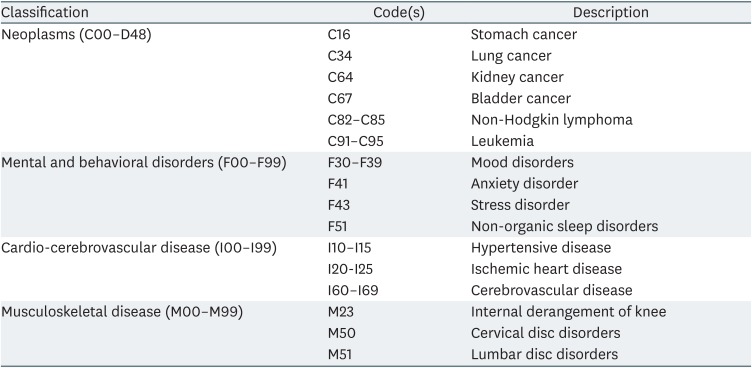
We extracted the number of people with disease in 2017 from the NHIS database. Because the selected diseases of cancer, cardio-cerebrovascular disease, mental disorders, and musculoskeletal disease are chronic, we considered a 7-year time gap between getting qualification of job entitled at 2010. We selected diseases by the main categories of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10). We selected the middle categories of ICD-10, and in the category of neoplasms, we selected stomach cancer (C16), lung cancer (C34), kidney cancer (C64), bladder cancer (C67), non-Hodgkin's lymphoma (C82–C85), and leukemia (C91–C95). For mental and behavioral disorders, we selected mood disorders (F30–F39), anxiety disorder (F41), stress disorder (F43), and nonorganic sleep disorders (F51). In ICD-10 the definition of stress disorder is “reaction to severe stress, and adjustment disorders” (F43). For cardio-cerebrovascular disease, we included hypertensive disease (I10–I15), ischemic heart disease (I20–I25), and cerebrovascular disease (I60–I69). For musculoskeletal disease, we chose internal knee derangement (M23), cervical disc disorders (M50), and lumbar disc disorders (M51). Lumbar disc disorder was categorized as M51, which is “other intervertebral disc disorders” in ICD-10, and includes thoracic, thoracolumbar, and lumbosacral disc disorders. All of our selections are summarized in Table 1.
Our calculation of the prevalence rates was based on the ICD-10 disease classification codes and was defined as the total number of persons who requested to use a diagnosis code at least once, regardless of outpatient basis or hospitalization. Medical expenditure was defined as the sum of outpatient expenditures, drug costs, and hospitalization fees.
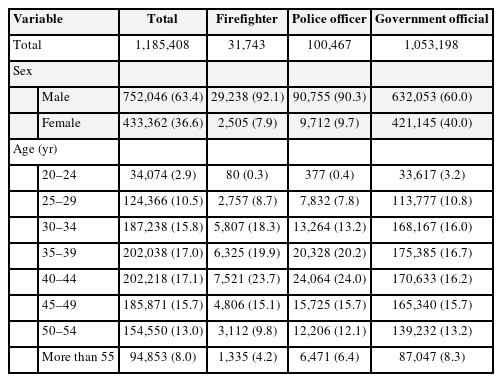
Accordingly, in our study there were 31,743 firefighters (29,238 men, 2,505 women), 100,467 police officers (90,755 men, 9,712 women), and 1,053,198 other government workers (632,053 men, 421,145 women).
Statistical analysis
Using data from select patients in the NHIS database in 2017, age-standardized prevalence rates were calculated by direct standardized method using Korean census data from 2010 as the standard population.
The medical expenditures of specific diseases were determined by dividing the total medical expenses related to a specific disease by the number of patients with each disease. The total medical expense per person was calculated as the sum of the respective medical expenditures. The total medical expenses were presented in US dollars using the 2017 currency exchange rate (1 USD = 1,130.61 KRW). Because the populations of the 3 groups were different, we calculated the age-adjusted medical expenditures using the direct standardized method based on the total number of individuals (firefighters, police officers, and government officials) as the standard population. All statistical analyses were performed using R.3.6.1.
Ethics statement
This study was approved by Institutional Review Board of Hanyang University (HY-18-10-16).
RESULTS
Demographics
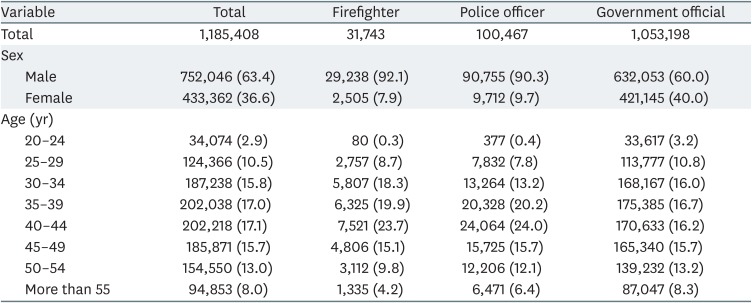
This study comprised 1,185,408 subjects in 3 job categories, most of whom were male (86%). Of the 31,743 firefighters, 28,238 were male (92%) and 2,505 were female (8%). Of the 100,467 police officers, 90,755 were male (90%) and 9,712 were female (10%). Of the 1,053,198 government officials, the proportion of males was 60%; the proportion of females was larger than in the firefighter and police groups. We calculated age-adjusted prevalence rates for the target populations (firefighters and police officers) and the general population (government officials); the results are summarized in Table 2.
Neoplasms
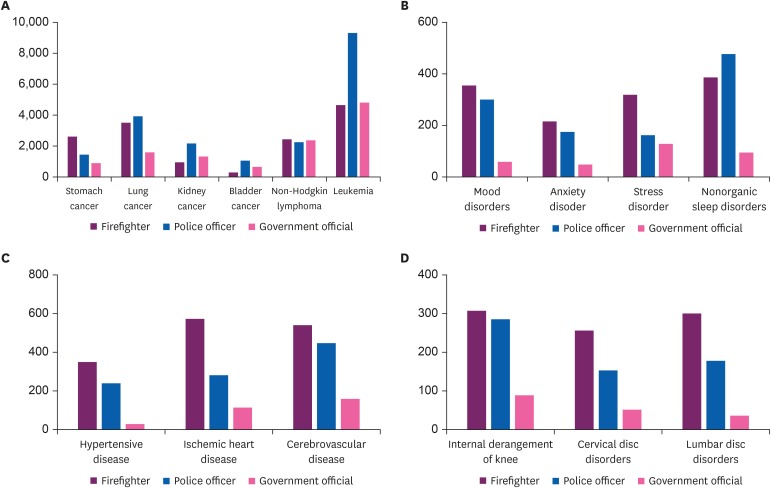
There were no significant differences in the age-adjusted prevalence for cancer between firefighters, police officers, and government officials (Supplementary Table 1, Fig. 1). As, medical expenditure, for males, only stomach cancer showed significant differences between job categories, after age adjustment. For female firefighters, no medical expenditure of cancer was significantly higher than in other jobs. For the total study population, firefighters did not show a significant difference in medical expenditure compared to the other 2 jobs (Supplementary Tables 2 and 3, Fig. 2).
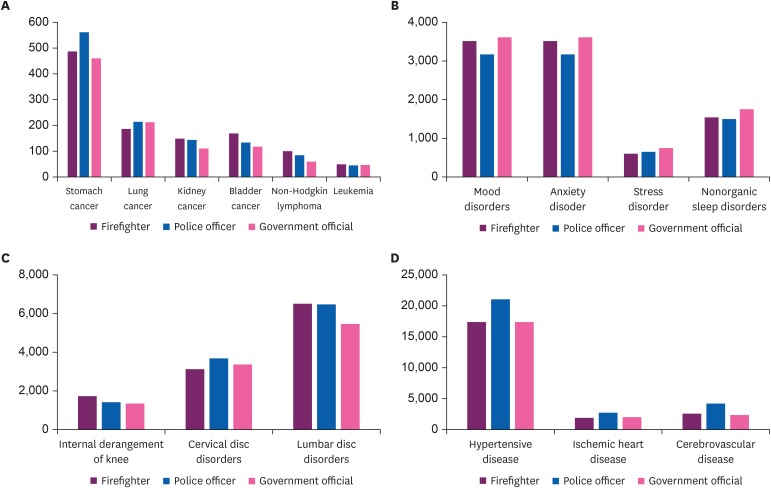
Age-adjusted prevalence of disease. Prevalence of (A) cancer, (B) mental disorder, (C) cerebrocardiovascular disease, and (D) musculoskeletal disease.
Vertical axis is prevalence of disease per 100,000.
Mental and behavioral disorders
There were no significant differences in age-adjusted prevalence for mental and behavioral disorders between the 3 job categories (Supplementary Table 1, Fig. 1). However, age-adjusted medical expenditures were different among the 3 jobs. Male firefighters spent 6.5 times more than government officials for mood disorders, 4.9 times more for anxiety disorders, and 4.5 times more for sleep disorders, after age adjustment. Female firefighters did not show significant differences in medical expenditures (Supplementary Tables 2 and 3, Fig. 2).
Cardio-cerebrovascular disease
For the firefighter population, the age-adjusted prevalence per 100,000 was not significantly different from that of government officials and police officers (Supplementary Table 1, Fig. 1). However, the medical expenditures related to cardio-cerebrovascular disease were quite different among the 3 occupations. Of the cardio-cerebrovascular diseases, medical expenditures for hypertensive disorders were relatively higher than for other diseases in this category (Fig. 2); the total medical expenses for hypertensive disorder for both sexes were 12.4 times higher than for government officials, and 1.5 times higher than for police officers (Supplementary Tables 2 and 3). For male firefighters, the medical expenses of every type of cardio-cerebrovascular disease (hypertensive disease, ischemic heart disease and cerebrovascular disease) were higher than for government officials and police officers. For female firefighters, only hypertensive disease showed a difference (Supplementary Table 3, Fig. 2).
Musculoskeletal disease
For the firefighter population, the age-adjusted prevalence per 100,000 population of musculoskeletal disease was not different from the other 2 occupations (Supplementary Table 1, Fig. 1). However, medical expenditures for every included disease (i.e., internal derangement of knee, cervical disc disorders, lumbar disc disorders) were higher for firefighters than for both police officers and government officials. Total medical expenses for lumbar disc disorders for both sexes of firefighters were 8.4 times higher than for government officials, and 1.7 times higher than for police officers (Supplementary Table 3, Fig. 2). For male firefighters, medical expenses related to every musculoskeletal disease were higher than for both government officials and police officers. Female firefighters spent more than the other groups for both cervical disc disorders and lumbar disc disorders (Supplementary Table 3, Fig. 2).
DISCUSSION
By using a nationwide database, our study determined that the prevalence of disease in firefighters was not significantly different from that of police officers and government officials. However, firefighters spent more money for health care than other 2 occupation groups. Apart from the age-adjusted prevalence, firefighters spent much more money than other groups on psychiatric disease, cardiovascular disease and musculoskeletal disease.
We compared the prevalence of cancer with the general population of Korea by the reported studies. For stomach cancer, age-standardized prevalence rate of male Koreans was 425.6 per 100,000 in 2016, and for lung cancer it was 110.2 per 100,000 in that same year [22]. Compared to that study, the prevalence for stomach cancer was high (firefighters 479.7 per 100,000, police officers 533.2 per 100,000, government officials 520.3 per 100,000). The age-standardized prevalence rates of bladder cancer, non-Hodgkin's lymphoma, and leukemia were, respectively, 64.1, 45.9, and 39.2 per 100,000 in 2016 [22]. Compared to that study, the prevalence for bladder cancer, non-Hodgkin’s lymphoma and leukemia were relatively high. According to a previous study on the economic burden of disease in Korea in 2015, that for stomach cancer was $2,283 million USD [23]. According to another cohort study for which the data source was NHIS, the total average cumulative medical expenditure for 5-year lung cancer patients ranged from $11,273 USD to $19,054 USD [15]. Compared to that study, the total medical expenditures for lung cancer in our study was low (firefighters $3,279 USD, police officers $2,816 USD, government officials $1,115 USD).
To compare firefighters with the general population, the age proportion had to be considered. Initially, we intended that the government officials cohort would represent the general population, but we learned that this group did not have the same characteristics as the general population. Among the 3 groups, there was no significant difference in cancer prevalence or medical expenditures. Prevalence of lung cancer, which was expected to be high for firefighters, was slightly lower than that of the other 2 groups [4]. In the case of cancer, only the medical expenses of stomach cancer were higher than for both government officials and police officers. Because we targeted actively working groups (defined as persons having occupations in 2010 and 2011 consecutively), terminal-stage cancer patients could be omitted. Furthermore, firefighters retire at 60 years of age, so, unlike the general population, the age range of firefighters was from 20 to 60 years. Due to this limited age range and typical disease characteristics, cancer patients tend to quit or lose their jobs after diagnosis and so might have been excluded from our population [24].
For mental and behavioral disorders, firefighters paid more than both government officials and police officers, actually 2.6 to 6.8 times more than government officials. For mood disorders, firefighters spent 6.1 times more than government officials, and 4.1 times more for sleep disorders; the comparison to police officers was similar. Both firefighters and police officer had high medical expenditure of sleep disorder. We assumed that shift work schedules could aggravate sleep disorders. Firefighters' total medical expenditures for anxiety disorders was 4.4 times higher than government officials, and 1.2 times more than that of police officers.
The prevalence of mental disorders among firefighters was lower than in the general population [25]. For the general population in 2011, the lifetime prevalence of mood disorders was 4.8%, and of anxiety disorders was 5.3% [25]. For several categories of sleep disorders, the prevalence in the general population ranged from 4.9% to 19.0% [26]. Compared to the general population, the prevalence of all of studied psychiatric diseases, mood disorder, anxiety disorder, stress disorder and nonorganic sleep disorder among firefighters was low. For the general population, the median cost of mood disorders was $1,391 USD, $620 USD for stress disorders and anxiety disorders, and $913 USD for sleep disorders [27]. Firefighters' medical expenditures of most psychiatric disease were lower than that of the general population. This could be explained by the fact that we targeted actively working groups, so that severe disease conditions might have been excluded. Nevertheless, compared to the general population, firefighters' medical expenditures for sleep disorders was similar to the general population. This meant that, considering the age proportions, firefighters' sleep disorders were much worse than the general population.
In the cardiovascular and cerebrovascular disease category, firefighters' expenditures for every specific disease (hypertensive disorder, ischemic heart disease, and cerebrovascular disease) were significantly higher than both government officials and police officers (Supplementary Table 1). For example, compared to government officials, firefighters spent 12.4 times more for hypertensive disease, 4 times more for ischemic heart disease, and 3.3 times more for cerebrovascular disease. For musculoskeletal disorders, firefighters' medical expenditures for lumbosacral disorders were much higher than that of police officers and government officials. For lumbar disc disorders, they spent 8.4 times more than government officials and 1.6 times more than police officers (Supplementary Table 3, Fig. 2).
There are 2 important implications in these results. First, the severity of disease might be different in different occupational groups. It is easier to cure diseases, not only cancer but also psychiatric disease, at their early stage [2829]. However, as a disease becomes chronic it becomes more severe, making it harder to cure and more expensive [28]. Previous study has shown that catastrophic or high medical expenditures could result in unmet medical needs, which could result in exacerbation of disease and occurrence of complications [30]. Such considerations must be included in evaluation of health care provision [30]. We supposed that differences of health expenditure could reflect unmet medical needs in the early disease stages. However, this was difficult to conclude based on use of indirect data sources and lack of information on economic status.
According to a previous study on firefighters, the frequency of leaving the job because of health problems was 60% higher than in other industry workers [31]. For firefighters, diseases of the circulatory system, musculoskeletal diseases, and mental disorders were the main reasons for both sick leave and disability retirement [31].
In their fire suppression work, firefighters bear higher physical loads than do office workers, including carrying, kneeling, squatting, pulling, and walking stairs [32]. Due to higher metabolic demands for firefighting tasks, the risk of cerebrovascular disease is higher in firefighters [7]; in previous studies, firefighters' risk of both angina pectoris and myocardial infarction was higher than for government officials [7]. For the same reasons, firefighters have a higher risk of moderate musculoskeletal disorders, as they have greater physical strength and incur more accidents than the general population [10].
As for mental illness, for firefighters the prevalence and medical expenditures were higher than for police officers; the prevalence rate was similar to that of government officials, but the medical expenditures were higher. In addition, the high frequency of verbal and physical assaults could increase the risk of heart disease or cerebral hemorrhage [33]. When firefighters battle a fire at a major disaster site, they can encounter traumatic events, possibly leading to PTSD [12].
Second, these results reflect the importance of routine health check-ups for firefighters as well as follow-up management. This information could be used for developing health care policies for firefighters. Firefighters in Korea are obligated to have annual health check-ups, but this is controversial [34]. A previous study showed that health check-ups were not effective in changing health-related behaviors [35], and therefore post-check-up management programs are now recommended for improving their effectiveness. Especially after routine check-ups, at-risk groups and actual patients should be managed systematically and effectively.
Our study had some limitations. First, it was based on NHIS data, which is actual patient data from hospitals rather than estimated data [36]. Because the data was collected for medical services claims and reimbursement, it was not optimized for diagnosis of disease [36]. Thus, even if it could represent the actual status of entire groups, the data used was not all-inclusive. For example, because we used mid-class codes of ICD-10, non-targeted diseases or trivial symptoms could have been included. The mid-class codes of ICD-10 are “families” of various diseases, such as “lumbosacral disc disorders” (the M51 code). This could also include cervical disc disorders with cervicalgia and cervico-thoracic disc disorders, which were not our target. Interpretation of our study results should note this context.
Second, because of insurance claim systems, we could not include non-reimbursed expenses or complementary and alternative medicine. According to a previous study, medical expenses are of 2 types, direct and indirect, and assessment of direct medical expenses calculates actual money that patients paid for drugs, outpatient care, and hospitalization fees [37]; this consists of reimbursed and non-reimbursed expenses [38]. In this study, we could only include reimbursed expenses; as a result, the medical expenditures described in this study could be underestimated. Also, we could not account for occupational information such as job tenure, type, and title due to lack of information in the claims data.
CONCLUSIONS
Nevertheless, our study has value in that it represents the exact scale of diseases within specified cohorts, because the study data was based on reported claims. There has not been much previous study on the medical expenditures of firefighters, but this study shows that this group has very significantly higher medical expenditures than the comparison groups, government officials and police officers, despite having similar disease prevalence. Therefore, appropriate systems should be established to manage diseases at the early stage, and to prevent disease, such as follow-up management for medical health examinations.
Notes
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Jang TW, Kim I, Song J, Koh SB.
Data curation: Kim HS, Min J.
Investigation: Min J, Kim Y, Han J.
Writing - original draft: Min J, Kim Y.
Writing - review & editing: Min J, Han J, Kim Y, Jang TW.
Abbreviations
CI
confidence interval
EMS
emergency medical services
HR
hazard ratio
ICD-10
10th revision of the International Statistical Classification of Diseases and Related Health Problems
NHIS
National Health Insurance Service
PTSD
post-traumatic stress disorder
References
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Age-adjusted prevalence of disease by jobs (per 100,000) in 2017
Supplementary Table 2
Medical expenditures of disease per person by jobs in 2017
Supplementary Table 3
Age-adjusted medical expenditure scale of disease in 2017