Relationship between long work hours and self-reported sleep disorders of non-shift daytime wage workers in South Korea: data from the 5th Korean Working Conditions Survey
Article information
Abstract
Background
Studies have investigated the relationship between long work hours and sleep disorders; however, they have focused on shift workers or specific workers who are at high risk of industrial accidents rather than wage workers in general. The purpose of this study is to investigate the effects of long work hours on sleep disorders among non-shift daytime wage workers.
Methods
We conducted a secondary analysis of data from the 5th Korean Working Conditions Survey. From the 50,205 total participants, we included 26,522 non-shift daytime wage workers after excluding self-employed people, business owners, unpaid family employees, and wage workers who work nights and shifts. Sleep disorders were categorized into “difficulty in falling asleep,” “frequent waking,” and “waking up with fatigue.” Logistic regression analysis was used to evaluate the influence of long work hours on sleep disorders, and the odds ratios (ORs) were calculated.
Results
The OR of working > 52 hours per week was 1.183 (95% confidence interval [CI]: 1.002–1.394) for the risk of developing insomnia compared with working ≤ 40 hours per week. The OR of waking up with fatigue was 1.531 (95% CI: 1.302–1.801). Long work hours showed no significant relationship with difficulty in falling asleep or with frequent waking.
Conclusions
Working for extended hours was associated with increased fatigue upon waking in non-shift daytime wage workers.
BACKGROUND
Workers in South Korea worked an average of 1,993 hours per year in 2018, which is well above the average of 1,734 hours reported by the Organization for Economic Cooperation and Development for member countries [1]. The legal work hours in South Korea were changed to 40 hours per week in 2003. However, with 12 hours of overtime work and holiday work, it was possible to work up to 68 hours per week. Since July 1, 2018, a maximum limit of 52 hours of work per week has been legally enforced for public institutions and companies with 300 or more employees. Starting in 2020, this rule was extended to workplaces with 50 or more employees. However, 5 special-purpose industries, including healthcare and transportation, are not covered by this regulation to shorten work hours [2]. Despite legal restrictions, some individuals are still working long hours.
Health problems caused by long work hours have been studied previously and include a number of conditions, such as circulatory diseases, diabetes, metabolic syndrome, depression, anxiety, and sleep problems [3]. According to the International Labor Organization, sleep disorders, regardless of the cause, have an adverse effect on health; they increase the risk for diabetes and cardiovascular diseases (such as dyslipidemia, and hypertension), and of early mortality by 40% [45]. Previous studies have investigated the relationship between long work hours and sleep disorders, but they have focused on shift workers or specific workers who are at high risk of industrial accidents, rather than wage workers in general [67]. And there is a lack of research on the detailed items of sleep disorders with regard to work hours [8].
In this study, we investigated whether long work hours, excluding shift work and night work, affect sleep conditions. Furthermore, this study was conducted to ascertain which type of sleep disorder is specifically associated with long work hours. Shift work and night work are strongly related to sleep disorders, and they are also associated with long work hours in South Korea [9]. Thus, even if a statistical correction is performed, it would likely cause residual confounding [10]. Therefore, this study only examined daytime workers to exclude possible effects of night or shift work on sleep disorders.
METHODS
Study participants
This study comprises a secondary analysis of data from the 5th Korean Working Conditions Survey (KWCS) (2017), conducted by the Occupational Safety and Health Research Institute (OSHRI) of the Safety and Health-Policy Research Department in South Korea. The KWCS benchmarked the European Working Condition Survey (EWCS) and the Labor Force Survey of the United Kingdom to understand the overall work environment, such as work patterns, employment type, occupation, industry, exposure to risk factors, and employment stability, among workers older than 15 years in South Korea. The study population of the KWCS comprised employees (age > 15 years) who lived in households based on the 2010 Population and Housing Census [11] and who had worked for more than an hour for the past week for “income.” The KWCS includes information on the characteristics of approximately 50,000 workers. To collect the data, professional survey agents visited the participants' homes and conducted face-to-face interviews [12].
Among the 50,205 participants included in the 5th KWCS, we excluded self-employed people, business owners, and unpaid family employees, because their labor characteristics and circumstances differ from those of wage workers. Among the remaining 30,232 wage workers, those who worked night or shift work were also excluded. The remaining 26,522 workers were enrolled in this study. To increase the reliability of the analysis, weights were applied, and the number of participants after weighting was 32,861. The weights were calculated by the raking-ratio method in OSHRI [13].
Operational definition of factors
Dependent factors
Until the 4th KWCS, there had not been any specific investigations on insomnia; The 4th KWCS only collected information about whether there were insomnia or sleep-related problems in the preceding 12 months. From the 5th KWCS, the survey on sleep-related problems was further refined into 3 categories by referring to the EWCS as follows: “difficulty in falling asleep,” “waking up repeatedly during sleep (frequent waking),” and “waking up with a feeling of exhaustion and fatigue (waking without feeling refreshed).” These items were scored on a 5-point Likert scale and were classified based on their frequency into “daily” (4 points), “several times a week” (3 points), “several times a month” (2 points), “less often” (1 point), and “never” (0 points). “Daily” (4 points) and “several times a week” (3 points) were classified as indicating sleep-related problems; several times a month (2 points), less often (1 point), and never (0 points) were classified as indicating no sleep-related problems. The total scores of the 3 categories were 0 to 12. Scores of 6 and below indicated no insomnia, and scores of 7 and above indicated insomnia. Scoring was based on the median value.
Personal characteristics
The personal characteristics of the study participants included classified as sex, age, education level, monthly income, subjective health condition, disease or health problems, depression, and anxiety.
Education levels were classified dichotomously as “high school or below” and “college or above.” The average monthly income was classified into 4 sections, referring to the income quintile standard of urban working households in South Korea, simplifying the 9-group classification by the 5th KWCS. Respondents were asked “How is your health in general? Would you say it is very good, good, fair, bad, or very bad?”. “Very good” and “good” were classified as “good,” “fair” was classified as “fair,” and “bad” and “very bad” were classified as “bad.” The presence of disease was ascertained through “yes” or “no” answers to the question “Do you have any illness or health problem which has lasted, or is expected to last, for more than 6 months?” Respondents were also asked about depression and anxiety. They replied either “yes” or “no” to the question “Over the last 12 months, did you have any of the following health problems?”
Occupational factors
The occupational characteristics analyzed in this study included weekly work hours, duration of the service, size of the workplace, type of occupation, and commuting time. The weekly work hours were classified into ≤ 40, 41–52, and > 52 hours according to the Labor Standards Act. The legally permissible work hours in Korea are 40 hours a week, and overtime work is limited to 12 hours. However, in exceptional industries, workers could work for > 52 hours. Therefore, working for > 52 hours was defined as long work hours in this study. The duration of service was classified into < 1, 1–5, 6–10, and > 10 years. The types of occupations were simplified into white-collar workers (managers, experts and related workers, and office workers), pink-collar workers (service workers and sales workers), and blue-collar workers (skilled agricultural, forestry, and fishery workers; craft and related workers; equipment/machine operating and assembling workers; elementary workers; and those in the armed forces). Commuting time was defined as the sum of the time taken to go to work and return home and was classified into 4 categories. Workplaces were classified by their size into small-scale workplaces (< 50 employees), medium-scale workplaces (50–249 employees), and large-scale workplaces (≥ 250 employees), based on the European Union classification criteria [14].
Statistical analysis
For the statistical analysis of the research data, we used SPSS ver. 25.0 (SPSS Inc., Chicago, IL, USA); Frequency analysis was conducted for the personal and occupational characteristics of the participants. The χ2 test was used to assess the association of sleep disorders with the participants' characteristics. Logistic regression analysis was performed to evaluate the influence of working hours on sleep-related problems, and odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. The statistical significance level was set at p < 0.05. OSHRI recommends the application of weights when analyzing KWCS raw data, because the KWCS sampling design is that of a secondary probability proportion-stratified cluster-sample survey that can cause significant bias if the weighted values are not applied in the statistical analysis. Therefore, we used weighted data to show the number of people, overall proportions (%), and the p-values.
RESULTS
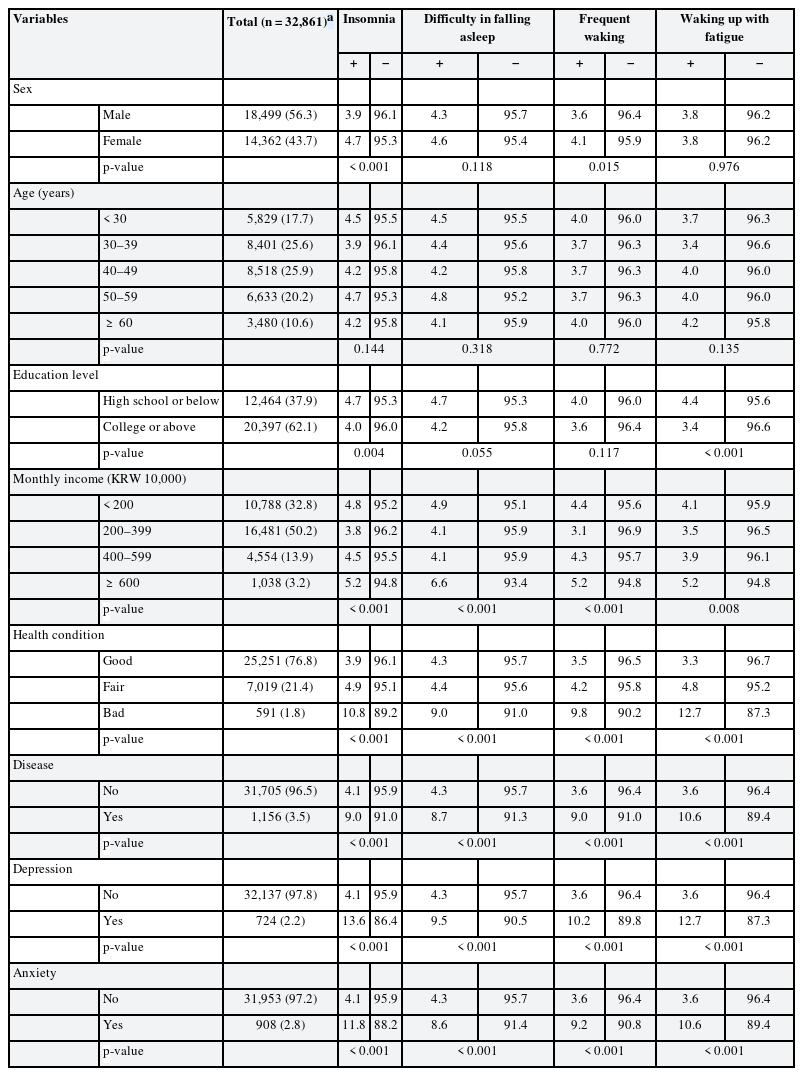
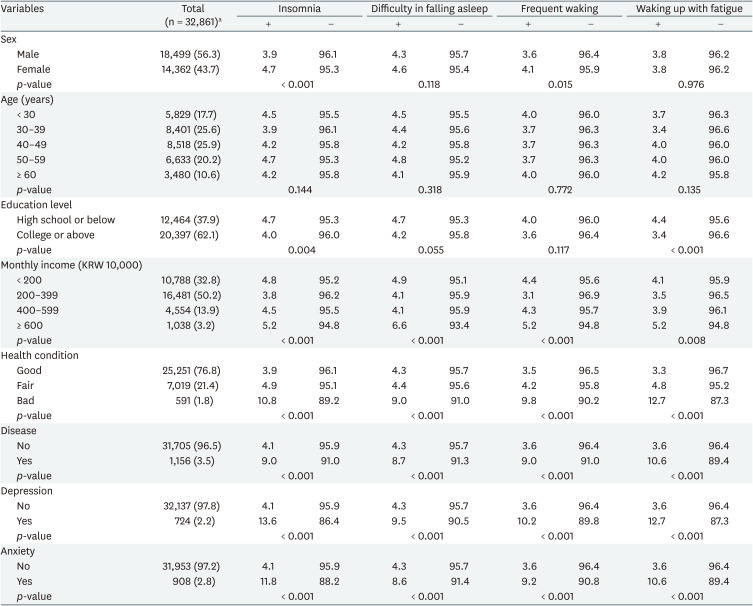
Relationship between participants' characteristics and sleep disorders
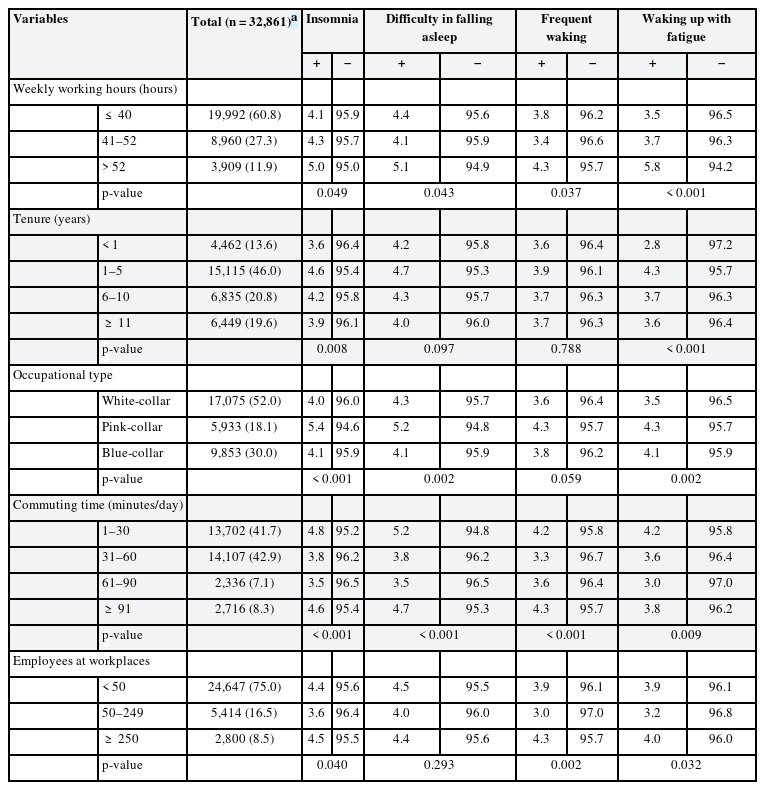
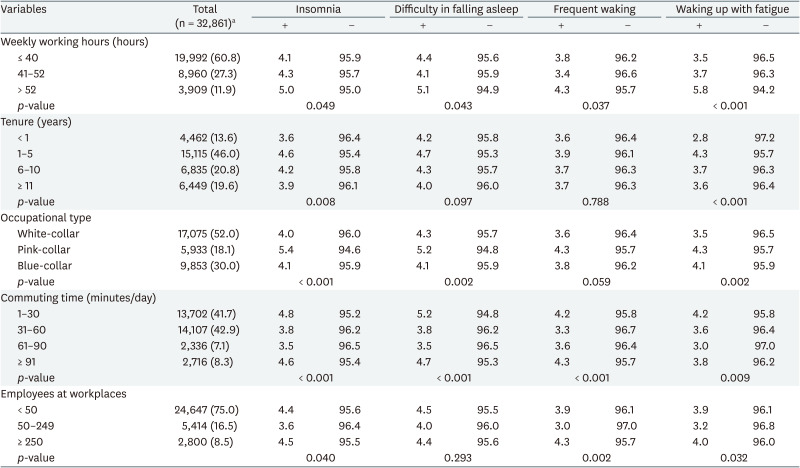
The group with disease was more than twice as likely (9.0%) to experience insomnia than was the group without disease (4.1%), which was statistically significant (p < 0.001). In the group experiencing depression, 13.5% experienced insomnia, which was more than 3 times higher than the 4.1% rate of insomnia in the non-depressed group and the difference was statistically significant (p < 0.001; Table 1). In the group of participants who worked ≤ 40, 41–52, and > 52 hours per week, 4.1%, 4.3%, and 5.0%, respectively, experienced insomnia, and the difference was statistically significant (p = 0.049). The group of participants who worked > 52 hours showed higher proportions of sleep-onset disorder, sleep-maintenance disorder, and waking without feeling refreshed, and the intergroup differences were statistically significant (p = 0.043, p = 0.037, and p < 0.001, respectively; Table 2).
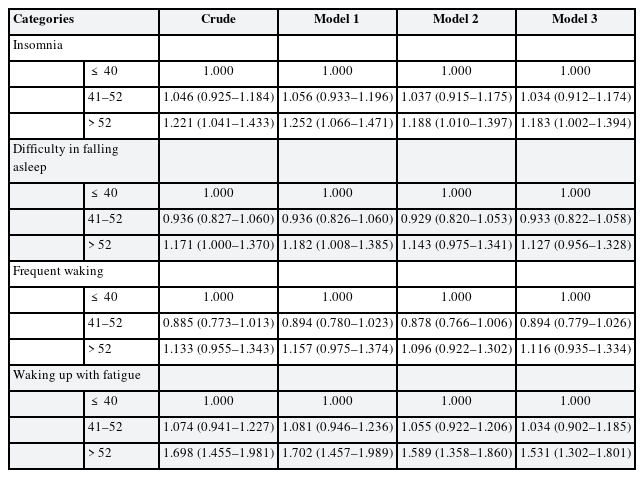
Relationship between participants' weekly working hours and sleep disorders
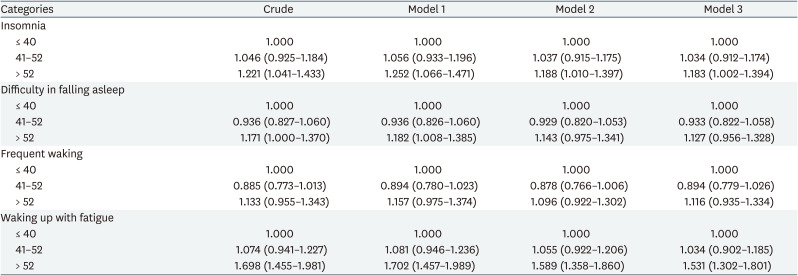
After adjusting the variables related to sleep disorders, we performed logistic regression analysis. Compared to participants who worked ≤ 40 hours per week, the OR for developing insomnia was 1.183 (95% CI: 1.002–1.394) in participants working > 52 hours per week, and the difference was statistically significant. The OR for developing insomnia was 1.034 (95% CI: 0.912–1.174) for participants working 41–52 hours per week, but the difference was not statistically significant. An evaluation of the risk of sleep disorders from working > 52 hours in subgroup analysis by sleep disorders showed OR 1.531 (95% CI: 1.302–1.801) for waking without feeling refreshed. The risk of waking without feeling refreshed was highest for those with long work hours and was statistically significant. However, the OR decreased when adjusted for additional variables compared with the OR of 1.702 (95% CI: 1.457–1.989), which was only adjusted for sex and age. The ORs for sleep-onset disorder and sleep-maintenance disorder were 1.127 (95% CI: 0.956–1.328) and 1.116 (95% CI: 0.935–1.334), respectively. Findings for sleep-onset disorder were similar to those for waking without feeling refreshed; when only sex and age were adjusted, there was a significant increase in the proportion of participants who worked > 52 hours per week, but the statistical significance disappeared when dependent variables of other personal and occupational characteristics were also adjusted (Table 3).
DISCUSSION
The results showed that the risk of insomnia increased with long work hours, and it was possibly caused by a significant increase in the incidence of waking without feeling refreshed, rather than by sleep-onset or sleep-maintenance disorders.
There was a similar, previous study on the effect of long working hours on sleep disturbances in public officials in the United Kingdom with similar characteristics of non-shift daytime workers [15]. Our findings are similar to those of the UK study, but there is a slight difference. In the UK study, long working hours mainly caused “sleep-onset disorder,” whereas in this study, they mainly caused “waking without feeling refreshed.” This is presumed to reflect socio-cultural differences in the way people spend time after work. In addition, the participants in the 2 studies were public officials and daytime wage workers, with different occupational characteristics. Therefore, it seems that the job-related differences between a specific job group and all workers were reflected. Caruso et al. [16] stated that long work hours affect sleep time, recovery time from work, and the utilization of personal time. A probable causal relationship between long work hours and sleep disorders can presumably be attributed to poor recovery because of the lack of leisure time after work. At the end of the workday, workers may need a certain amount of time to recover from fatigue caused by the work effort. Because longer work hours increase the need for recovery from work [17], workers need more time to recover, which can hamper sleep time.
Previous studies have shown that sleep disorders are highly associated with psychological disorders, particularly mood, anxiety, and substance related disorders [1819]. In this study, sleep disorders were more common in the group that experienced depression and anxiety than in other groups. Furthermore, these mental illnesses were related to poor recovery following long work hours. Poor recovery can cause occupational burn out, which can lead to mental illnesses, thereby resulting in sleep disorders. The results of this study support this theory [20]. It is unclear whether insomnia is a primary disease or a symptom of a mental disorder; however, according to previous studies, 30%–50% of patients with insomnia had coexisting mental disorders, such as depression and anxiety disorder [18]. However, the assessment of the association between sleep disorders and mental disorders was beyond the scope of this study and is a task for a future study. Although our study did not analyze the link between long work hours and physical illness, we can partially explain the findings of this study in that long work hours increased the risk of waking with a feeling of exhaustion and fatigue, based on past research that long work hours are associated with physical illness [321].
This study did not fully explain the relationship and causality between work hours and sleep disorders, but it strengthened the evidence from existing studies in determining that long work hours are associated with sleep disorders [82223]. In addition, each of the 3 detailed causes of sleep disorders was analyzed to identify which aspects of sleep disorders are associated with long work hours.
Summarizing the aforementioned results, long work hours can cause health problems such as sleep disorders; therefore, active preventive management, such as strengthening occupational safety and health, is needed for groups working long hours. This study focused on non-shift workers who have been less studied compared to shift workers, including night shift workers. Moreover, the study is meaningful in that it reflects the reality of South Korean wage workers by using the data from the KWCS.
This study has some limitations. First, the KWCS has the limitation of being a cross-sectional study and did not select the variables reflecting the characteristics of each occupation. Second, this study did not investigate the relationship between long work hours and insomnia by sex and age. Third, we controlled the effects of various confounding or mediating factors; however, because of the lack of data, we could not control for the effects of smoking, alcohol, caffeine and drug abuse. Fourth, because of the lack of data on sleep time, the objective correlation between sleep time and subjective appeal to sleep problems was not discernable. Finally, the presence of sleep disorders, which was the dependent variable in this study, was based on answers about whether respondents had experienced sleep-related problems over the past 12 months. The KWCS uses a self-reporting method, and the interpretation of the results of our study should consider the reliability of self-reports of work hours and sleep disorders.
CONCLUSIONS
We found that long work hours of non-shift daytime wage workers were associated with increased fatigue when waking up in our evaluation of sleep disorders.
Acknowledgments
We would like to thank the Safety and Health Policy Research Department (Occupational Safety and Health Research Institute [OSHRI]) for offering the raw-data of the Korean Working Conditions Survey (KWCS). The paper's contents are solely the responsibility of the author and do not necessarily represent the official views of the OSHRI.
Notes
Funding: This work was supported by the Soonchunhyang University Research Fund.
Competing interests: The authors declare that they have no competing interest.
Availability of data and materials: The source of data is the 5th Korean Working Conditions Survey (KWCS; 2017), Occupational Safety and Health Research Institute (OSHRI).
Author Contributions:
Conceptualization: Choi H, Min YS.
Data curation: Min YS.
Investigation: Choi H, Min YS.
Writing - original draft: Choi H.
Writing - review & editing: Min YS, Lee S, Jeon MJ.
Abbreviations
CI
confidence interval
EWCS
European Working Condition Survey
KWCS
Korean Working Conditions Survey
OR
odds ratio
OSHRI
Occupational Safety and Health Research Institute