Association between sleep duration and impaired fasting glucose according to work type in non-regular workers: data from the first and second year (2016, 2017) of the 7th Korean National Health and Nutrition Examination (KNHANE) (a cross-sectional study)
Article information
Abstract
Background
We aimed to find the relationship between sleep duration and impaired fasting glucose according to working type in non-regular workers using the 2016 and 2017 Korean National Health And Nutrition Examination (KNHANE, 7th revision).
Method
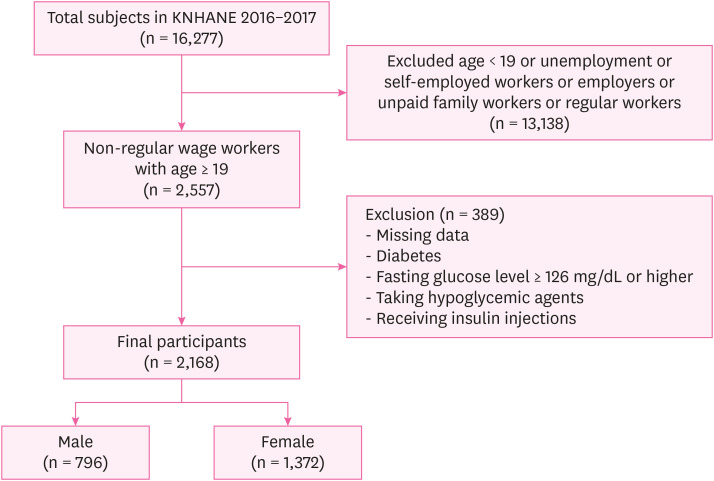
In the 1st and 2nd year (2016, 2017) of the 7th KNHANE, 16,277 people participated. Minors were excluded because this study was intended for individuals aged 19 years and older. As this study was based on wage workers, unemployment, self-employed workers, employers, unpaid family workers, and those who have insufficient answers such as unknown or no response were excluded. Regular workers were excluded because this study was intended for non-regular workers. Finally, a total of 2,168 people were included in the survey, except those who had been diagnosed with diabetes, had a fasting blood glucose level of 126 mg/dL or higher, or taking hypoglycemic agents or receiving insulin injections. To find the relationship between sleep duration and impaired fasting glucose according to work type in non-regular workers, multiple logistic regression analysis was performed by adjusting the general and occupational characteristics after stratification according to work type. All statistical analyses were performed using the SPSS software (version 26.0; SPSS Inc., Chicago, IL, USA).
Results
In the case of insufficient sleep duration in irregular female workers, the odds ratio (OR) of impaired fasting glucose was statistically insignificant, but in the case of insufficient sleep duration in irregular male workers who have shift work, the odds ratio (OR) of impaired fasting glucose was significantly higher than that of sufficient sleep duration (Model 1, OR: 3.05, 95% confidence interval [CI]: 1.18–7.90; Model 2, OR: 2.81, 95% CI: 1.08–7.29).
Conclusions
Our findings demonstrate that insufficient sleep duration was associated with an increase in fasting blood glucose levels in non-regular male workers working shifts. This means that non-regular workers are in desperate need for adequate sleep and health care. We hope that our study will help improve the health of non-regular workers and more systematic and prospective follow-up studies will be conducted to further improve the health of non-regular workers.
BACKGROUND
Since the 1997 financial crisis, the surge in non-regular workers due to labor cost reduction and restructuring has been a serious social problem. According to the data released by the Statistic Korea in October 2019, as of August 2018, non-regular workers accounted for 36.4% of all wage workers, the highest level since 36.6% in 2007 [1]. The increasing number of non-regular workers can lead to income inequality and job instability, which can have a negative impact on the psychological health, motivation to work, and job satisfaction of individuals. In addition, it has a significant impact on family members [234]. According to previous studies, people with lower occupational classes are more likely to work in harsh environments, including shift work, air pollution, and low job control ability. The low occupational class here means physical work, where the proportion of non-regular workers is higher than that of regular workers [5]. Previous studies have reported that non-regular work increases the risk of health problems due to excessive drinking and smoking and death from various cancers and other causes [67].
Shift work, including night shifts, disrupts the circadian rhythm and can cause many problems [89]. Many studies have evaluated the effects of shift work on health. Shift work can increase the incidence of digestive system symptoms, including indigestion and stomach ulcers, resulting from sleep disorders and dietary changes. In addition, it increases the risk of glucose metabolism abnormalities, obesity, and hyperlipidemia, thereby increasing the risk of cardiovascular diseases. Furthermore, the rate of spontaneous abortion, premature birth, and breast cancer may be increased in women working night shifts [1011].
According to the Organization for Economic Co-operation and Development (OECD) statistics, the average daily sleep duration for Koreans is 7 hours and 41 minutes, which is 41 minutes short of the OECD average of 8 hours and 22 minutes, making it the lowest daily sleep duration reported among OECD countries [12]. This includes weekends and non-working days; therefore, the average sleep duration is expected to be lower on weekdays and working days. Adequate sleep duration plays an important role in appetite regulation, immune regulation, endocrine function, and glucose metabolism [13]. Previous studies have reported a significantly higher risk of metabolic syndrome in groups with less than 6 hours of sleep per day on average [14]. In addition, insufficient sleep duration can lead to weight gain, increase insulin resistance, and blood glucose disorders, one of the diagnostic criteria for metabolic syndrome, as well as increase the incidence of type 2 diabetes [15]. Moreover, overseas studies have reported that sleep deprivation increases the incidence of chronic diseases and mortality, and decreases quality of life [16].
Impaired fasting glucose (pre-diabetes) is defined as a fasting glucose level of 100–125 mg/dL, which is measured after 8 hours of fasting among those who have never been diagnosed with diabetes by a doctor [17]. Globally, the number of diabetes patients is expected to increase rapidly from 1.7 billion in 2000 to 3.7 billion by 2030 [18]. According to the Diabetes Fact Sheet in Korea 2018 presented by the Korean Diabetes Association, as of 2016, 1 in 7 adults (14.4%) had diabetes, and the prevalence of diabetes has increased for 6 years since 2011. As of 2016, 31.0% of men aged more than 30 years and 19.7% of women aged more than 30 years had impaired fasting glucose levels [19]. Previous study reported that people diagnosed with impaired fasting glucose were 1.5 times more likely to develop type 2 diabetes than normal people within 10 years [20]. In addition, persons diagnosed with impaired fasting glucose can have diabetes for only 3 years unless their blood sugar levels remain high even after making certain lifestyle changes [20]. Diabetes is one of the leading causes of cardiovascular mortality, including diabetic retinopathy, chronic renal disease due to diabetic nephropathy and neuropathy [21]. According to a recent study, in people with impaired fasting glucose, the risk of cardiovascular disease was 1.18 times higher than normal people [22]. According to another study, in men, no significant association was observed between cardiovascular disease and impaired fasting glucose; in women, the risk of cardiovascular disease was 1.7 times higher in those with impaired fasting glucose [23].
Several studies investigated the association between sleep duration and diabetes [24]. Although some studies examined the association between sleep duration and impaired fasting glucose [25], the number of studies is limited. Moreover, Korean studies on the association between sleep duration and impaired fasting glucose are insufficient, especially among non-regular workers. Therefore, this study aimed to investigate the relationship between sleep duration and impaired fasting glucose according to sex and work type among non-regular workers aged 19 years and older.
METHODS
Study participants
This study used the 2016 and 2017 Korean National Health And Nutrition Examination (KNHANE, 7th revision). The KNHANE is a national representative statistical survey on national health and nutritional status conducted by the Korea Centers for Disease Control and Prevention under the Ministry of Health and Welfare. The statistics and data collected through this survey will be used to establish health policies and programs and conduct research for the promotion of national health. A total of 192 areas were included in the survey, and 23 sample households were selected using the system extraction method; meanwhile, facilities such as nursing homes, military, prisons, and foreign households were excluded from the survey. Within the sample households, all household members aged 1 year and older who met the requirements for appropriate households were selected for the survey. In the 1st and 2nd year (2016, 2017) of the 7th KNHANE, 16,277 people participated. Minors were excluded because this study was intended for individuals aged 19 years and older. As this study was based on wage workers, unemployment, self-employed workers, employers, unpaid family workers, and those who have insufficient answers such as unknown or no response were excluded. Regular workers were excluded because this study was intended for non-regular workers. Finally, a total of 2,168 people were included in the survey, except those who had been diagnosed with diabetes, had a fasting blood glucose level of 126 mg/dL or higher, or taking hypoglycemic agents or receiving insulin injections (Fig. 1).
Measurement
General and occupational characteristics
The participants' general characteristics included age (< 30 years, 30–39 years, 40–49 years, 50–59 years, and ≥ 60 years), education (≤ elementary school, middle school, high school, ≥ and college), body mass index (BMI) (< 25 normal or ≥ 25 overweight), hypertension and hypercholesterolemia (yes or no), alcohol consumption (≤ once a month and ≥ twice a month), and smoking status (never-smoker, ex-smoker, or current smoker). The occupational characteristics included physical labor status (non-physical, physical), weekly working hours (≤ 52 hours or > 52 hours), monthly income (< 1,000,000 Korean won [KRW], 1,000,000–< 2,000,000 KRW, 2,000,000–< 3,000,000 KRW, or ≥ 3,000,000 KRW), and work type (daytime work or shift work).
Sleep duration
In accordance with the 7th KNHANE, daily sleeping hour was divided into the following categories: weekdays (or working day) average daily sleeping hours and weekends (or non-working day, the day before no work) average daily sleeping hours from average daily sleeping hours regardless of weekdays and weekends. The participants were asked to respond to the question, “What time do you go to bed and wake up during the weekdays (or working days)”: sufficient if the sleep duration is more than 6 hours and insufficient if the sleep time is 6 hours or less [26].
Impaired fasting glucose levels
In a blood test, a fasting glucose level of 100 mg/dL is considered normal, while a level of 126 mg/dL or more indicates impaired fasting glucose [17].
Statistical analyses
First, a χ2 test was used to determine the distribution of irregular workers with impaired fasting glucose according to their general and occupational characteristics. Next, the χ2 test was used to determine the distribution of impaired fasting glucose according to sleep duration. Then, the study analyzed the relationship between sleep duration as an independent variable and impaired fasting glucose as a dependent variable. After stratifying according to the work type in each man and woman, a logistic regression analysis was performed by adjusting the general and occupational characteristics. In the unadjusted model (Model 1), a univariate logistic regression analysis was performed to determine the association between sleep duration and impaired fasting glucose levels. In the second model, a multiple logistic regression analysis was performed by adjusting the occupational characteristics (weekly working hours, physical labor status, and monthly income). In the third model, a multiple logistic regression analysis was performed by adjusting the general characteristics (age, alcohol, smoking, BMI, hypertension, and hypercholesterolemia). In the fourth model, a multiple logistic regression analysis was performed by adjusting the general characteristics (age, alcohol, smoking, BMI, hypertension, and hypercholesterolemia) and occupational characteristics (weekly working hours, physical labor status, and monthly income). The significance level was set at 0.05. All statistical analyses were performed using the SPSS software (version 26.0; SPSS Inc., Chicago, IL, USA).
RESULTS
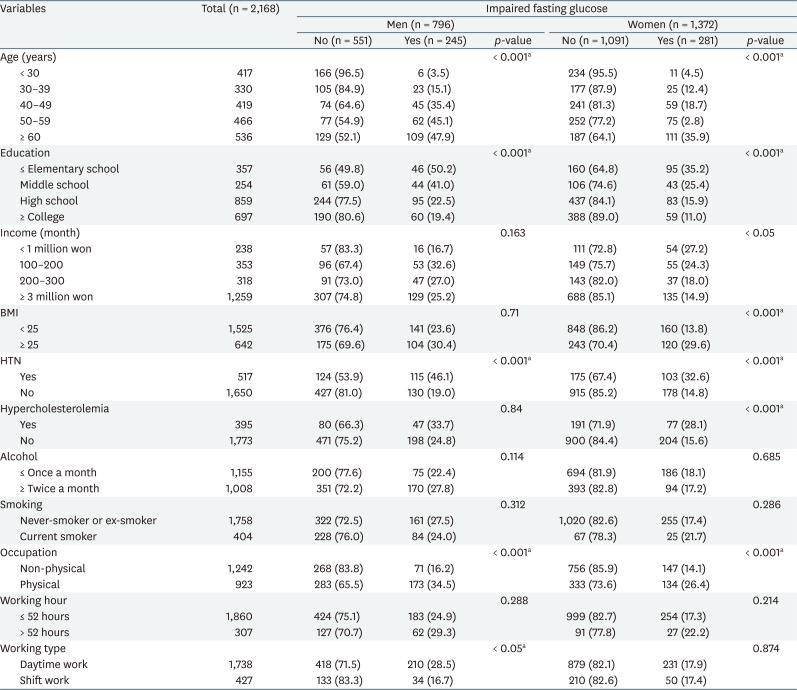
Distribution of impaired fasting glucose according to general and occupational characteristics
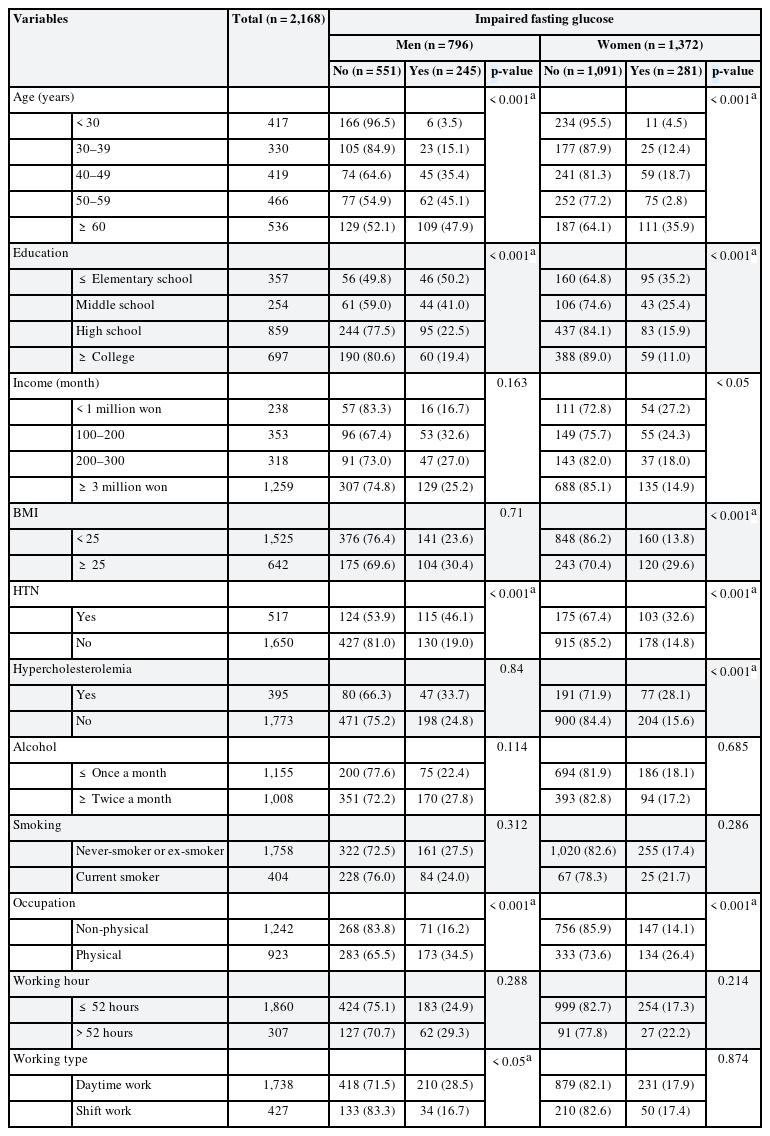
In both men and women, the higher the age and the lower the education level, the higher the incidence of impaired fasting glucose. In women with high BMI, the incidence of impaired fasting glucose was high; in men, impaired fasting glucose and BMI showed no significant difference. In both men and women with hypertension, the incidence of impaired fasting glucose was significantly high. In women with hypercholesterolemia, the incidence of impaired fasting glucose was high; however, in men, no significant difference was observed between hypercholesterolemia and impaired fasting glucose. No significant difference was observed in the incidence of drinking and smoking between men and women. In women, a lower monthly income was associated with higher incidence of impaired fasting glucose; however, in men, no significant difference was observed between monthly incomes and impaired fasting glucose. In both men and women, in the case of physical labor, the incidence of impaired fasting glucose was high, but no significant difference was observed between weekly working hours and impaired fasting glucose. In men, the incidence of impaired fasting glucose was high among shift workers. In women, no significant difference was observed between impaired fasting glucose and shift work (Table 1).
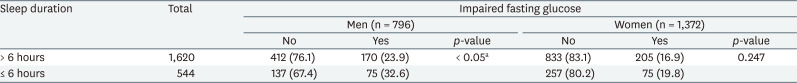
Distribution of impaired fasting glucose according to sleep duration
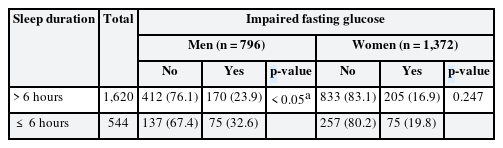
In men with insufficient sleep duration, the incidence of impaired fasting glucose was high. However, in women, no significant difference was observed between insufficient sleep duration and impaired fasting glucose (Table 2).
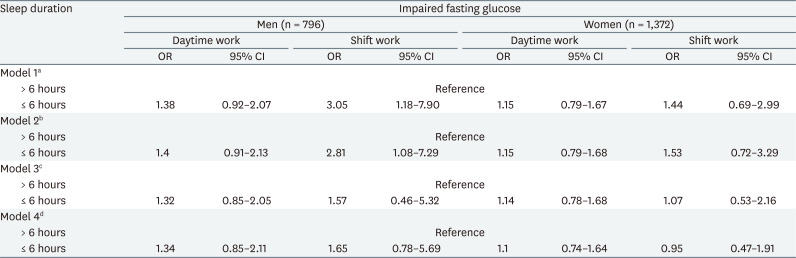
Relationship between sleep duration and impaired fasting glucose according to work type
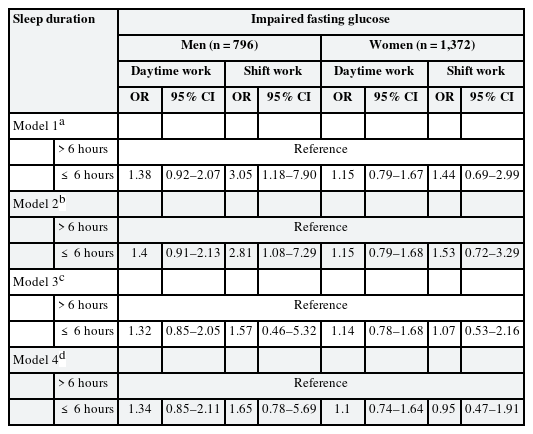
In models 1 and 2, in the case of insufficient sleep duration in irregular male workers who have shift work, the odds ratio (OR) of impaired fasting glucose was significantly higher than that of sufficient sleep duration (Model 1, OR: 3.05, 95% confidence interval [CI]: 1.18–7.90; Model 2, OR: 2.81, 95% CI: 1.08–7.29) (Table 3).
DISCUSSION
The study found what relationship sleep duration had with impaired fasting glucose of non-regular workers in both men and women.
In this study, the correlation between short sleep duration and impaired fasting glucose was significant when the occupational characteristics were adjusted in men. However, the correlation between short sleep duration and impaired fasting glucose was insignificant when the general and occupational characteristics were adjusted. Previous studies investigating the association between short sleep duration and blood glucose disorders in men reported conflicting results. In an 8-year prospective study of 2,649 adult male workers in a Japanese electrical company who had never had diabetes or other chronic diseases, the association between sleep disorders and type 2 diabetes was statistically significant after adjusting for age, education, occupation, shift work, BMI, leisure time physical activity, smoking, alcohol consumption, and family history of diabetes [27]. According to Kim et al., in the group with less than 7 hours of sleep per day, the odds ratio between short sleep duration and impaired fasting glucose was 1.46 (95% CI: 1.08–1.96) compared with the group with 7–8 hours of sleep per day after adjusting for age, BMI, education level, monthly income, marital status, smoking, alcohol, regular physical activity, and stress recognition in 5.868 men aged 19 years and above [28]. However, Choo et al. [29] reported that there was no significant association between short sleep duration and diabetes in the group with less than 6 hours of sleep per day after adjusting for age, BMI, smoking, drinking, exercise, stress, and melancholy in 7,036 adult men compared with 6–8 hours of sleep per day. Previous studies reported the association between sleep duration and impaired fasting glucose according to work type [30]. However, it is difficult to directly compare the results of our study with those of previous studies as none of them examined the relationship between sleep duration and impaired fasting glucose in non-regular workers. In addition, there are no studies that have evaluated the association between short sleep duration and impaired fasting glucose levels by adjusting the occupational characteristics. As shown in previous studies, the association between sleep duration, impaired fasting glucose, and diabetes in adult men is inconsistent. The results of this study showed that there was a significant correlation between lack of sleep duration and impaired fasting glucose after adjusting for occupational characteristics in male non-regular workers. This finding suggests that insufficient sleep duration may cause impaired fasting glucose in non-regular workers.
There are several biological mechanisms in which insufficient sleep duration can adversely affect blood glucose metabolism. First, sleep deprivation can lead to changes in the neuro-hormonal regulation of feeding behavior. Previous studies have shown that sleep deprivation can increase the appetite-stimulating hormone “ghrelin” and appetite-suppressing hormone “leptin,” which can cause changes in feeding behavior and thus lead to weight gain and obesity [3132]. Sleep deprivation can lead to obesity, which can increase the prevalence of diabetes [33]. In another mechanism, sleep deprivation activates the sympathetic nerve, resulting in increased cortisol secretion at night. This mechanism increases insulin resistance, suppresses pancreatic function, and reduces blood glucose tolerance [3435]. These neuroendocrine changes interfere with glucose control and eventually increase the blood glucose levels [36]. In addition, activation of inflammatory pathways due to sleep deprivation may play an important role in inhibiting glucose metabolism. Previous studies have reported that sleep deprivation is associated with increased tumor necrosis factor alpha, interleukin-6, and C-reactive protein [3738]. Furthermore, these inflammatory factors are important predictors of type 2 diabetes [3940].
For women in this study, there was no significant association between sleep duration and impaired fasting glucose regardless of work type in non-regular workers. Looking at previous studies investigating the association between sleep duration and blood glucose disorders in women, a 10-year follow-up of 70,026 women who had never been diagnosed with diabetes in the United States Nurses' Health study found that the risk of developing diabetes in those with less than 5 hours of sleep was 1.57(95% CI: 1.28–1.92) [41]. However, a 32-year follow-up study of 1,462 Swedish women reported no association between insufficient sleep duration and diabetes [42]. In addition, a 12-year follow-up study of 2,663 men and women aged 45–65 years in Sweden showed that sleep duration of less than 5 hours was reported to increase the risk of diabetes in men but not in women [43]. These results support our findings, which indicate that there is no significant association between sleep duration and impaired fasting glucose in women. According to Roehrs et al., the prevalence of sleep-related respiratory disturbance is higher in men than in women; even though sleep-related respiratory disturbance is adjusted, sleep efficiency is still low in men [44]. According to Engeda et al. [45], who evaluated 2,285 adults aged more than 30 years who had never been diagnosed with sleep disorders, those with low quality of sleep and short sleep duration had higher risk of pre-diabetes compared with those who had 7–8 hours of sleep per day. For this reason, the association between sleep duration and impaired fasting glucose may increase in men. According to Heianza et al. [46], who investigated the association of menopause with type 2 diabetes and pre-diabetes in 6,308 pre-menopausal women and 4,570 post-menopausal women in Japan, menopausal state was significantly associated with type 2 diabetes and pre-diabetes compared with pre-menopausal state. This finding suggests that menstruation also has an important effect on blood glucose levels in women.
To date, many studies have evaluated the association between sleep duration and diabetes [47484950]. In addition, several studies have reported that shift work can increase the risk of diabetes [5152]. However, only a few studies have investigated the association between sleep duration and impaired fasting glucose according to work type. To the best of our knowledge, this is the first study to examine the association between sleep duration and impaired fasting glucose by sex and work type in non-regular workers.
This study has some limitations. First, as a cross-sectional study, it is difficult to elucidate the temporal relationship between sleep duration and the incidence of impaired fasting glucose. However, KNHANE is a nationwide date that represents a country, we believe that it can aid in the design of future studies that related to non-regular workers. Second, the subdivisions of KNHANE's sleep-related survey into the weekday (or working day) and weekend (or non-working day, the day before no working) were introduced from the 7th KNHANE. Therefore, we targeted only the samples of first and second year of 7th KNHANE. However, we had significant results so we believe that further research will be needed when more data is accumulated in the future.
One strength of this study is that it is the first study in Korea to evaluate the relationship between sleep duration and impaired fasting glucose according to the type of work for non-regular workers using KNHANE. A previous study examined the association between sleep duration and impaired fasting glucose according to the type of work, but was not conducted among non-regular workers. Therefore, this study is meaningful as it suggests the importance of health care among non-regular workers. The second KNHANE is a nationwide survey using a large sample size. In addition, it is a comprehensive study that evaluates the social and economic level, location, lifestyle, and health conditions of individuals. Therefore, it is a significant data representing a country.
CONCLUSIONS
In this study, the relationship between sleep duration and impaired fasting glucose was examined according to the type of work in non-regular workers. Our findings demonstrate that insufficient sleep duration was associated with an increase in fasting blood glucose levels in non-regular male workers working shifts. Our study shows that non-regular workers are in desperate need for adequate sleep and health care. Sufficient sleep duration can effectively lower the fasting blood glucose levels. Furthermore, impaired fasting glucose indicates pre-diabetes and thus can lower the risk of developing type 2 diabetes. Finally, we hope that more systematic and prospective follow-up studies will be conducted to further improve the health of non-regular workers.
Notes
Funding: This work was supported by the research fund from Soonchunhyang University.
Competing interests: The authors declare that they have no competing interest.
Availability of data and materials: This study used data from the 7th Korean National Health And Nutrition Examination (KNHANE), which is open for any researchers after request. All study participants of the KNHANE agreed to participate the survey and signed an informed consent.
Author Contributions:
Conceptualization: Lee J, Joo J.
Data curation: Joo J, Lee JG, Kim S, Lee J.
Formal analysis: Lee J, Joo J.
Writing - original draft: Joo J.
Writing - review & editing: Lee KJ, Lee J.
Abbreviations
BMI
body mass index
CI
confidence interval
HTN
hypertension
OECD
The Organization for Economic Co-operation and Development
OR
odds ratio
KNHANE
Korean National Health And Nutrition Examination