Risk factors including night shift work of colorectal polyp
Article information
Abstract
Background
The destruction of circadian rhythms by night shift work affects major circadian genes, which are known to play a role in advancing or killing the cell cycle through tumor suppressor genes. To find out whether night shift work affects the incidence of colorectal cancer, which was found to be associated with long-term night shift work in previous studies, we surveyed effect of night shift work on colorectal polyps that have a higher incidence than colorectal cancer and can progress to colorectal cancer.
Methods
To examine the correlation between rotating night shifts and colorectal polyps, a survey was conducted with 299 men aged 40–60 years from two university hospitals. We examined lifestyle, work history, work patterns, and colonoscopy results. The differences in prevalence among the groups was compared, and prevalence ratio (PR) was calculated via generalized linear modeling.
Results
The prevalence of colorectal polyps in night shift and non-shift workers were 53.0% and 33.5%, respectively. After adjusting for age, smoking status, dietary habits, family history of colorectal cancer, obesity, job type, night shift work (PR: 1.13, 95% CI: 1.02–1.25) was a risk factor of colorectal polyps.
Conclusions
The risk of colorectal polyps was greater in night shift workers than non-shift workers. Also risk of colorectal polyp was higher in older group. Our study investigated colorectal polyp instead of colorectal cancer and lacks information about types and gene mutations of colorectal polyps. Further study is needed to clarify effect of night shift work on development of colorectal cancer.
BACKGROUND
The incidence of colorectal cancer has recently increased in Korea. In 2017, the incidence of colorectal cancer was 30.8 per 100,000 people - the second most common cancer following stomach cancer. There were 28,111 cases of colorectal cancer; of these, 16,653 cases were men. Compared with other countries, the age-standardized incidence rate of all cancers in men was 291.3 in Korea, 285.9 in Japan, 393.2 in the US, and 344.7 in the United Kingdom. Specifically, Korea had a higher incidence of colorectal cancer (38.8) than other countries except Japan (49.1), including the US (28.8) and the United Kingdom (37.8). In women, the age-standardized incidence rate of all cancers was 251.5 in Korea, 220.5 in Japan, 321.2 in the US, and 299.8 in the UK. Specifically, the incidence of colorectal cancer was 21.8 in Korea, 29.6 in Japan, 22.6 in the US, and 27.0 in the UK, showing that females in Korea had a relatively lower incidence of colorectal cancer compared to other countries [12].
The relative risk of colorectal cancer was 1.35 (95% CI: 1.03–1.77) in the group with more than 15 years of shift work experience compared to the group with under 1 year of shift work experience in a cohort study of US female nurses [3]. Further, in a 24-year follow-up cohort study from 1988–2012 and from 1989–2013, the risk of colorectal cancer was 1.15 (95% CI: 0.95–1.39) and the risk of rectal cancer was 1.60 (95% CI: 1.09–2.34) in the group with more than 15 years of shift work experience [4].
Light exposure from night shifts reduces serum melatonin levels, and melatonin increases the expression of p53, a tumor suppressor gene [5]. Therefore, light exposure during night shifts may reduce the expression of tumor suppressor genes by decreasing serum melatonin production and may affect the circadian genes itself. Night shift working increases the risk of breast cancer owing to abnormalities in the hypothalamic-pituitary-gonadal axis by the effects of melatonin, a hormone that is secreted and suppressed under the influence of light [6]. Melatonin is also involved in the development of cancer by inducing cell proliferation and apoptosis through circadian genes in peripheral tissues through the hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes [7]. In addition, two circadian regulatory genes, Per2 and Per1 regulate β-catenin and cell proliferation in colon and non-colon cancer cells, and Per2 mutations make intestinal β-catenin and colorectal polyp formation increase [8]. There has been ample research concerning breast cancer and circadian rhythm genes [910].
According to the 2017 Korean Working Conditions Survey, since 2006, the proportion of workers working in shifts has been steadily increasing. According to the 5th Working Environment Survey, the proportion of shift workers accounted for 9.7%; of which 10.0% were men and 9.3% were women [11]. Further, based on the results of epidemiological studies and animal studies on breast cancer from the World Health Organization's International Agency for Research on Cancer (WHO IARC), it was concluded that shift work that disrupts the circadian rhythm is risk factor for developing cancer [12]. In 2019, though there was debate on effect of night shiftwork on risk of colorectal cancer, IARC maintained night shift work as probable carcinogen of breast, prostate and colorectal cancer [13].
Compared with other countries, the incidence of colorectal cancer in men is higher in Korea. In addition, Korean male workers have a higher rate of shift work. Therefore, we choose the group exposed to the risk of night work and colorectal cancer as the target of our study. Since night shift work could affect the incidence of colorectal cancer, we tried to indirectly determine whether night shift work is a risk factor for colorectal cancer by comparing the prevalence of colorectal polyp with other known risk factors of colorectal cancer [14], which is higher than colorectal cancer and is a precancerous lesion of colorectal cancer.
METHODS
Study setting and participants
The study protocol was reviewed and approved by the institutional Review Board of the Dongguk University Ilsan Hospital (approved No 2011-61) and Ulsan University Hospital (approved No 2011076). We examined the questionnaires and colonoscopy results of 476 men those who took informed consent among all the people who received a colonoscopy and 40–60 years old men during a health promotion examination in 2011 and 2012 at 2 University hospitals. Total 476 men were surveyed in our study. We excluded 177 individuals with answers including missing variables. As a result, data from total 299 participants was analyzed in this study.
Variables and instruments
Sociodemographic and work-related characteristics
We surveyed General characteristics and known risk factors of colorectal cancer included height, weight, age, sex, smoking, drinking habits, dietary habits, exercise habits, sleeping habits, and sleep disorders, family history of colon cancer by self-reporting questionnaires. We also investigated the presence of shift work, number of nightshifts, the type of shift work, and the level of activity at work. When men worked shift work, sleeping habits according to the work type were included in the survey. Abdominal obesity was defined as the waist circumference of more than 90 cm. Obesity was classified when their body mass index (BMI) was greater than 25 kg/m2.
We defined night shift work group as a group where the number of night work (work performed at least 2 hours between 10 pm and 5 am) exceeded 3 times per month. The definition of night work in the Working Conditions Survey Report in Korea was used [11]. Cut-off value of night work was previously used for a study on the link between breast cancer and night shift work in Germany in the past [15]. Day worker and those who do night shift work less than 4 times per month were classified no night shift work group.
Average daily sleeping time was calculated via individual's sleeping time when working daytime shifts and sleeping time when working nighttime shifts.
Colonoscopy results
Participants' colonoscopy results were collected after health examination and classified as normal, colorectal polyp, colorectal cancer, and other (including hemorrhoids, colitis, diverticulum).
Statistical analyses
A frequency analysis was performed using IBM SPSS Statistics software 25.0 (IBM, Armonk, NY, USA). Chi-square tests were used to determine the differences in prevalence among the groups, and t-tests were used for mean comparisons. In addition, due to high prevalence of colorectal polyp among current study population, Poisson regression model with robust error variance was used to determine the crude and adjusted prevalence ratio (PR) of colorectal polyps [16].
RESULTS
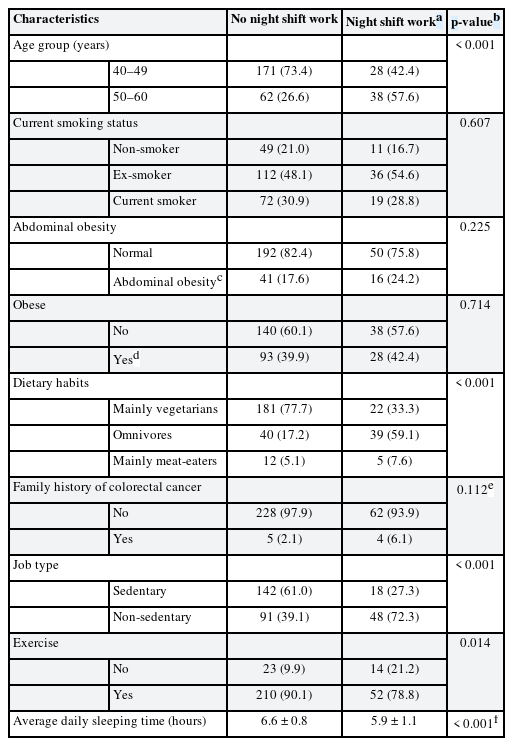
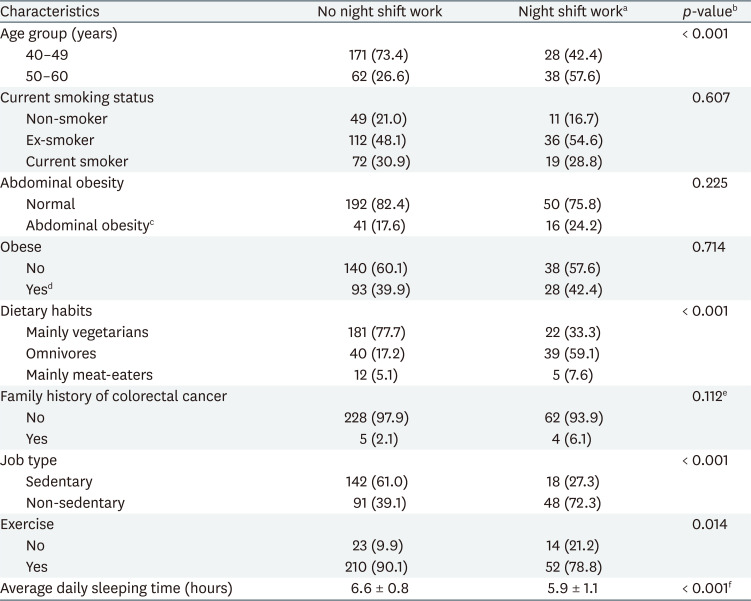
We compared the general characteristics of participants by night shift work in Table 1. The group with (vs. without) night shift work was older and active during work but did less exercise and the group without (vs. with) the night shift work was more likely to be mainly vegetarian. Also night shift work group had a shorter average daily sleeping time (5.9 hours vs. 6.6 hours). There was no significant difference between the groups concerning smoking rate, obesity, family history of colorectal cancer.
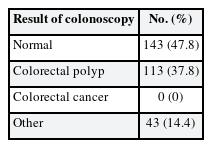
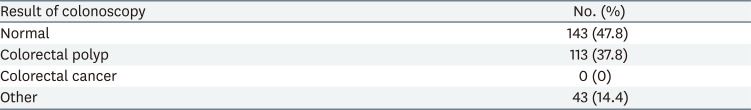
Table 2 shows colonoscopy result of our study population. There were no participants with colorectal cancer confirmed in the colonoscopy. All cases classified as other were hemorrhoids.
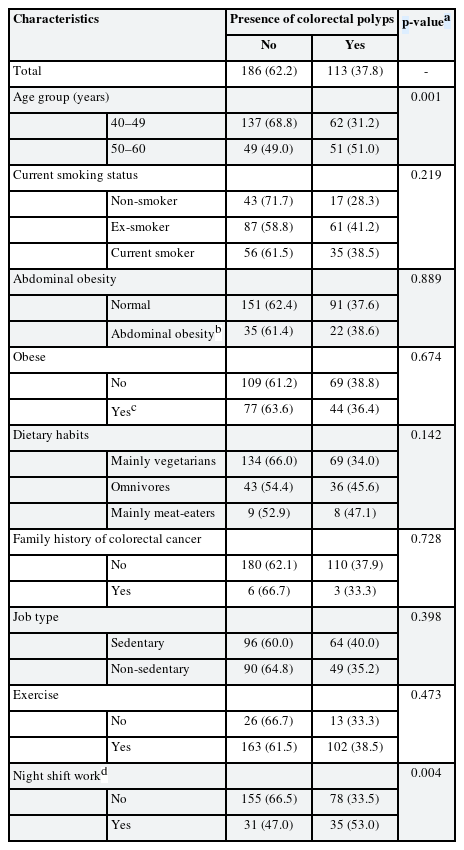
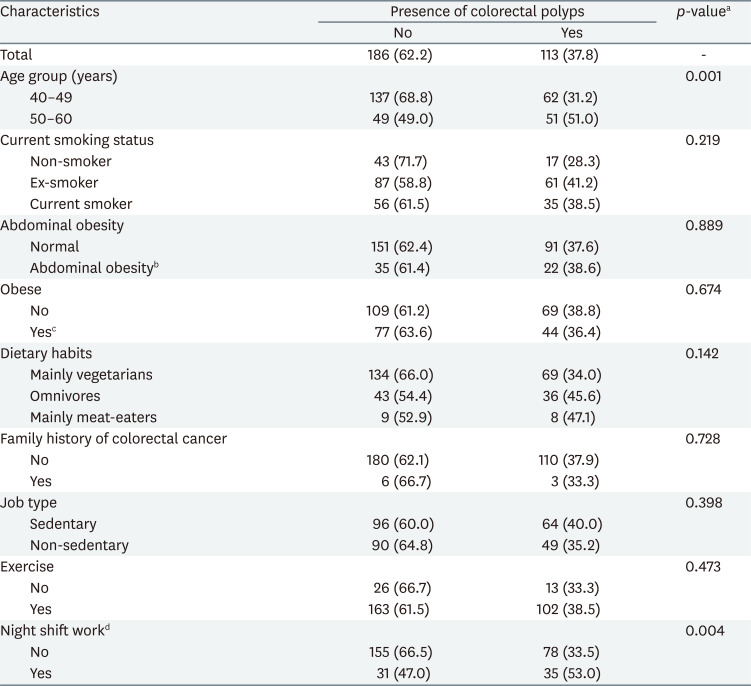
Table 3 shows participants' characteristics by the prevalence of colorectal polyps. The prevalence of colorectal polyps was significantly higher in those who work in night shift more than 4 times per month than those who work in night shift less than 4 times per month. The prevalence of colorectal polyps was significantly higher among older group. The other relationships were non-significant.
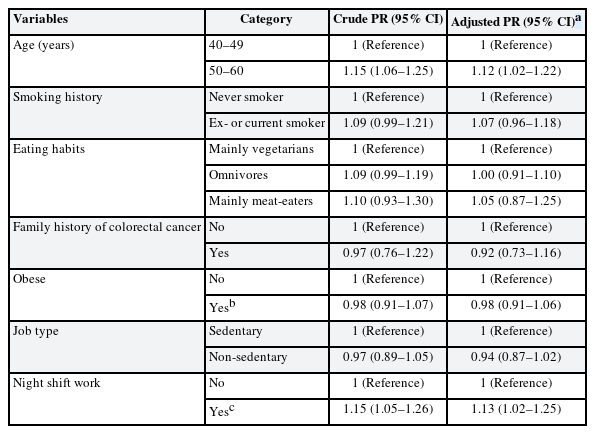
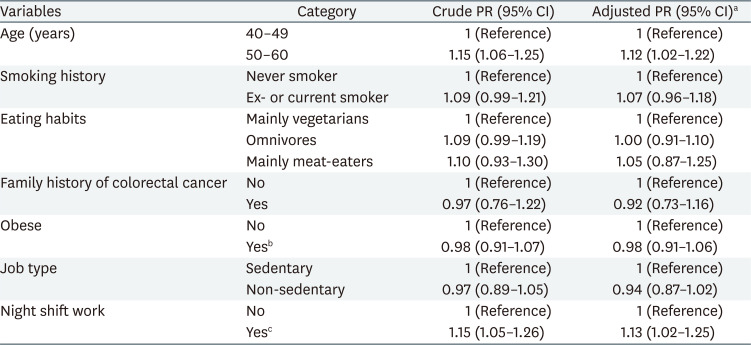
The PRs for the risk of colorectal polyps are shown in Table 4 with both crude ratios and ratios adjusted for age group, smoking status, dietary habits, family history of colorectal cancer, obesity, job type, and night shift work. In the analysis of individual variables, age (PR: 1.15, 95% CI: 1.06–1.25) and night shift work (PR: 1.15, 95% CI: 1.05–1.26) was significantly associated with elevated risk of colorectal polyps while other variables including smoking history, eating habits, family history of colorectal cancer, obese and job type was not significant. In the multivariable analysis including whole variables above, age (PR: 1.12, 95% CI: 1.02–1.22) and night shift work (PR: 1.13, 95% CI: 1.02–1.25) remained associated with the elevated risk of colorectal polyps.
DISCUSSION
The purpose of this study was to investigate the relationship between night shift work and colorectal polyps using a survey and the colonoscopy results of men aged 40–60 years. The group that worked night shifts more than 4 times per month was more likely to have colorectal polyps after correcting for other risk factors such as age, smoking status, dietary habits, family history of colorectal cancer, BMI, and activity level at work. And old age was also a risk factor of colorectal polyps.
The prevalence of colorectal polyps varies widely by race and country. Previous study of asymptomatic average-risk Koreans showed that the prevalence of colorectal adenoma in age group of 40s and 50s was 28.1% and 38.1% [17]. Another study found that the prevalence of colorectal adenoma in asymptomatic Korean men with average risk was 27.9 in 40s and 36.8 in 50s [18]. In our study, the overall prevalence of colorectal polyp was 37.8% and according to age, the prevalence was 31.2% in 40s and 51.0% in 50s which is consistent with findings of former studies.
The prevalence of colorectal cancer increases with age. Because the risk of colorectal cancer begins to increase when people are in their 50s, the United States Preventive Service Task Force (2016) strongly recommends screening when individuals are aged 50–75 years [19]. The Canadian Task Force on Preventive Health Care (2016) and the Asia Pacific Working Group in Colorectal Cancer (2015) also recommend screening for colorectal cancer in asymptomatic adults aged 50–75 years [2021]. Hawkins and Ward report that polyps with microsatellite instability can cause colorectal cancer and that methylation of human mut-L homologue 1 (hMLH1) promoter is a crucial step in the progression to cancer [22]. Kim et al. [23] found that k-ras mutations were found in 31.1% of the 45 polyps analysis in Korea and that methylation of hMLH1 occurred in 64.4% of polyps, which may become precancerous lesions of colorectal cancer. In a study on the influence of lifestyle factors of colorectal cancer, the odds ratio of colorectal cancers according to age, after adjusting for family history, BMI, smoking, and drinking, was 1.12 (95% CI: 1.02–1.22), and the prevalence of colorectal polyps also increased with age [24]. In this study, the group with colorectal polyps was significantly older than the group without colorectal polyps. After adjusting for smoking, eating habits, family history of colorectal cancer, obesity, job style, and night shift work, aging was a significant risk factor for colorectal polyps.
Smoking is also a risk factor for colorectal polyps [252627]. In a previous meta-analysis, compared to non-smokers the risk of colorectal polyps in current smokers was higher [28]; and Kim et al. [29] showed that the risk of colorectal polyps was 2.12 (95% CI: 1.23–3.66) in ex-smokers and 2.22 (95% CI: 1.29–3.83) in current smokers compared to non-smokers after adjusting for age, calories, calcium level, alcohol, BMI, and physical activity. In current study adjusted PRs were 1.07 (95% CI: 0.96–1.18) in ever smokers compared to non-smokers, which was non-significant. In our study, the average age of the current smoker group was 47.0 years old, significantly lower than that of the past smokers and non-smokers 48.8 and 47.6 (p = 0.006). It is thought that the effect of smoking was reduced due to this difference in age among these groups which was shown above to increase risk of colorectal polyps.
A meta-analysis about obesity and colorectal cancer found that risk of colorectal cancer of overweight men (BMI: 25–29.9) was 1.26 (95% CI: 1.04–1.52) compared to the normal-weight men and risk of those that were extremely obese (BMI ≥ 30 kg/m2) was 1.71 (95% CI: 1.33–2.19) [30]. In a study of Koreans, the risk of colorectal cancer higher for the obese group compared to the normal group, showing obesity as a risk factor for colorectal cancer [31]. In addition, Kim et al. [32] found that the risk of colorectal polyps was higher for both men and women with abdominal obesity to their counterparts. The risk of colorectal polyps was for obese was higher compared to those in normal weight, suggesting that obesity is associated with an increased risk of colorectal polyps. In this study, the prevalence of colorectal polyps was slightly higher in those with abdominal obesity and obesity; however, this was non-significant, and the mean BMI of the group with and without polyps was the same. In both the obese and non-obese groups, the rate of usual exercise was 89.3% and 86.5%, respectively. It is possible that exercise had reduced the effect of obesity.
Wolin et al. [33] reviewed and meta-analyzed studies about physical activity and exercise in relation to the risk of colorectal polyps, and they found that the risk of colorectal polyps owing to physical activity in men was 0.81 (95% CI: 0.67–0.98); i.e., increased exercise led to a lower risk of colorectal polyps. In this study, the prevalence of colorectal polyps was lower in the group with a work environment that involved physical activity compared to those with sedentary tasks; however, this was non-significant. There is a possibility that the effect of night shift work may have reduced the protective effect of physical activity in workplace, as the proportion of night shift workers working on sedentary task is significantly lower than the proportion of non-night shift workers working on sedentary task.
Koushik et al. [34] analyzed 14 cohort studies and found that there was no significant correlation between vegetable-rich diet and risk of colorectal cancer nor between fruit-rich diet and risk of colorectal cancer. The meta-analysis by Johnson et al. [35] showed that the risk of colorectal cancer was higher in the group that consumed meat 5 times a week, lower when fruits were consumed more than three times a, and also lower when vegetables were eaten more than five times a day; thus, they identified the protective effects against colorectal cancer when fruits and vegetables were regularly consumed. In this study, eating habit was not a significant factor.
A family history of colorectal cancer is a risk factor colorectal cancer and colorectal polyps. In a prospective cohort study, the age-adjusted relative risk of colorectal cancer was higher for those with a family history than those without family history; and, for those aged younger than 45 years, the relative risk was much higher, suggesting that, especially with younger age, family history of colorectal cancer increases the risk of colorectal cancer [36]. In this study, family history was not a significant factor; this could be owing to the small sample size that had a family history of colorectal cancer.
Lastly, concerning whether night shift work is a risk factor for colorectal polyps, Papantoniou et al. [4] completed a 24-year follow-up cohort study from 1988 to 2012 and from 1989 to 2013. They found that the risk of colorectal cancer was the risk of colorectal cancer was 1.15 (95% CI: 0.95–1.39) and the risk of rectal cancer was 1.60 (95% CI: 1.09–2.34 in the group with more than 15 years of shift work experience compared to those without it. There was a meta-analysis conducted by Xiao et al. [37] that showed significant association between night shift work and increased risk of colorectal cancer. A case-control study in Spain found increased risk of colorectal cancer in ever performed rotating shift work group compared to day workers [38]. However, a study of Australian women workers showed that the risk of colorectal cancer in those that worked night shifts for over 7.5 years compared with those with no exposure to night shiftwork was 0.95 (95% CI: 0.57–1.58), indicating no significant relationship between shift work and colorectal cancer [39]. In our study, the prevalence of colorectal polyps in the group with and without night shift work was 53.0% and 33.5%, respectively. The risk of colorectal polyps after adjusting for age group, smoking, eating habits, family history of colorectal cancer, obesity, and job style was significantly higher for the group with night shift work. One study found those who sleep less than 6 hours per night had a increased risk of colorectal adenomas [40]. This is consistent with the results of the current study because short sleep time appeared in the night shift work group of our study (5.9 hours vs 6.6 hours, respectively). Patel et al. [41] found shorter duration of sleep was associated with increase in tumor necrosis factor alpha (TNF-α). and Kim et al. [42] found that increased plasma levels of TNF-α is associated with increased risk of colorectal adenoma. This increased risk of colorectal polyps in night shift workers could be explained by the decrease in melatonin due to night light exposure to night time workers and the mutations in circadian regulatory genes, PER2 related colonic polyp formation caused by circadian disruption [8]. and by increase of circulating inflammatory cytokine like TNF-α [42] due to shorter sleep duration [41].
Since this study employed a cross-sectional design, it has a limitation about causality which cannot be identified. In addition, although night shift work experience was identified, we failed to identify participants' total amount of night shift work and the type of night shift work. Moreover, small sample size of this study would be another limitation. Because of the small sample size, we investigated association between night shift work and colorectal cancer indirectly through colon polyps rather than directly through colon cancer. Our data is also lacking information about history of colorectal polyp removal, which is also a risk factor of development of subsequent colorectal cancer [43]. Furthermore, colon polyps differ in the probability of developing colorectal cancer according to the types of polyps such as adenomatous polyps and non-adenomatous polyps [44] and regarding previous studies that showed a link between night shifts and an increased risk of certain subsite colorectal cancers, our study has limitations in not examining the types of colorectal polyps and subsites. Also, there are known changes in genes are associated with the development of colorectal cancer, and the lack of investigation on these genes in our study will also be a limitation. However, our study has a strength that it is the first study on night shift work experience and colorectal polyps in Korea. In addition, the survey and the actual patients' colonoscopy results were linked throughout the study. Since the diagnostic test was conducted at the time of the study, the prevalence of colon polyps in study participants could be identified more accurately than by a simple survey. This is another strength of our research.
CONCLUSIONS
The risk of colorectal polyps was greater in night shift workers than non-shift workers. Risk of colorectal polyp was higher in older group. Considering the recent large-scale studies that show an increased risk of colorectal cancer in long-term shift workers, further studies which conducted in large-scale cohort design with detailed information about individual's night shift work and colon cancer's characteristics including types, subsites and gene mutations are essential to elucidate the relationship between night shift work and risk of colorectal polyps and risk of colorectal cancer.
Notes
Funding: This study was supported by Korea Medical Institute.
Competing interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Jeong KS, Yoo C, Ahn Y, Kim M.
Data curation: Um K, Park C.
Investigation: Yoo C, Kim M.
Writing - original draft: Um K, Park C.
Writing - review & editing: Um K, Park C, Jeong K.
Abbreviations
BMI
body mass index
CI
confidence interval
OR
odds ratio
PR
prevalence ratio
SD
standard deviation
TNF-α
tumor necrosis factor alpha