Association between employment status and sickness presenteeism among Korean employees: a cross-sectional study
Article information
Abstract
Background
Sickness presenteeism (SP) indicates “going to work while being ill.” The importance of SP has only recently been investigated, and the association between SP and employment status has been inconsistent across studies. Therefore, we conducted this study to explore the association between SP and employment status by using presenteeism propensity (PP), which can reflect the individual decision-making process.
Methods
The study population included employees participating in the 5th Korean Working Condition Survey. We analyzed data of only employees with at least one health event, which was calculated as the sum of SP and sickness absenteeism days. Employment status was grouped into 3 categories: stable employment, unstable employment (contract period ≥ 1 year), and unstable employment (contract period < 1 year). Survey-weighted logistic regression analysis was conducted to assess the association between employment status and PP (dichotomized as “≤ 0.5” and “> 0.5”).
Results
Unstable employees (contract period ≥ 1 year) had higher odds of PP than stable employees (odds ratio [OR]: 1.23, 95% confidence interval [CI]: 1.03–1.47), whereas unstable employees (contract period < 1 year) had lower odds of PP than stable employees (OR: 0.82, 95% CI: 0.71–0.96).
Conclusions
Employment status was associated with SP. Given the negative health impact of SP, social efforts, such as paid sick leave, are required to reduce SP and enhance the health status of unstable workers.
INTRODUCTION
Employees who encounter health problems face a dilemma between attending work despite illness or availing a sick leave. Sickness presenteeism (SP) indicates “going to work while being ill,” whereas sickness absenteeism (SA) refers to “taking a sick leave.” Both of these factors affect not only the health of employees but also the productivity of the companies they work for.
SA has been extensively studied because it can increase social costs due to employee health problems and their reduced productivity [1234]. In contrast, the importance and seriousness of SP has only recently been explored, particularly in Korea [5]. The average annual prevalence of SP ranged between 40% and 70% across studies in some Scandinavian countries [6789]. In a study conducted in the UK, this prevalence showed an upward trend [10]. These above mentioned studies demonstrate the importance of SP. A high prevalence of SP has a negative impact on an employee's physical and mental well-being, including manifestations of allergies, arthritis, diabetes, and depression [11]. Moreover, SP is linked to loss of productivity, poor team cohesion, and workplace accidents [12].
Several studies have revealed an association between SP and certain socioeconomic factors. Long working hours and other occupational stressors were associated with SP [13]. In cross-sectional studies, the prevalence of SP was associated with job insecurities, poor social support, high job demands, and sick leave policies [6141516]. Moreover, according to some prospective studies, the prevalence of SP was associated with perceptual or psychologic health problems [17]. However, an association between SP and employment status has been inconsistently reported in several of these studies.
In Korea, unstable employment has surged over a short duration in 1997 following the International Monetary Fund (IMF) financial crisis, which was accompanied by increased job insecurity, income inequality, and unfavorable working conditions that had a detrimental impact on the health of employees [1819]. Because of unfavorable working conditions and job insecurities, unstable employment could be associated with a higher prevalence of SP [520]. However, an association between employment status and SP was found only in few studies [7892122].
The inconsistent results could be explained by variations in the research methodology of the studies. An employee's decision of SP involves 2 steps: the first one involves generating a health complaint (health process), and the second pertains to choosing between SP and SA (decision process) [23]. Previous studies of the determinants of SP share certain theoretical assumptions about the employee's decision-making process, and focus only on episodes of SP. Assuming that the studied variables increase the likelihood of an SP, the likelihood of a replacement decision (SA) is expected to decrease. However, many potential variables were associated with SA and SP in the same direction [242526]. This could be explained by “double risk factors,” which affect both—the employee health process and the decision-making process [9]. For example, assume that the frequency of SP for older and younger workers was found to be the same, 4 days a year. From the conventional perspective of considering only the number of SPs, the 2 tend to have the same presenteeism. If the condition is added that the old man's SA is 6 days and the young man's SA is 1 day, the interpretation becomes different. Older people had more sick days, and attended 40% of sick days, whereas younger people were more likely to attended 80% of sick days. Here, the age was a double risk factor that increased both SP and SA [26]. And it is expected that there are other factors that make young people choose SP more such as attendance requirements [23]. Job insecurity differed between stable and unstable employees [19]. Furthermore, job insecurity was a “double risk factor” [7]. The above mentioned error could interfere with the results; therefore, this variable could hardly reflect the decision-making process accurately by the methodological approaches used in previous studies, wherein only episodes of SP are considered regardless of episodes of SA. Therefore, before the decision-making process is analyzed, employees without health complaints should be excluded from the analysis dataset. Participants in good health do not undergo a decision-making process, which needs to be considered before either SP or SA is selected [27]. Another method of analyzing the likelihood of SP selection is to use the presenteeism propensity (PP), which is the ratio of SP days to the total number of health events (or the sum of SP and SA days). A higher PP indicates that employees are more likely to attend work than to take a sick leave. Thus, PP is better than SP to identify factors in the decision-making process [2728]. Therefore, we aimed to explore the association between employment status and SP by using PP in this study. This contrasts with previous studies that have demonstrated the prevalence of SP under the premise that employees worked when sick, despite differences in the degree of the rate of SP in the overall health event [7892022].
METHODS
Study participants
We used data obtained from the fifth Korean Working Condition Survey (KWCS) conducted in 2017 by the Korea Occupational Safety and Health Agency. The fifth KWCS intended to investigate various working conditions of the Korean working population, and is comparable to the European Working Conditions Survey and the UK Labor Force Survey.
Overall, 50,205 employees participated in the 5th KWCS (the survey weighted sample size: 50,205) and 30,109 (the survey weighted sample size: 37,132) were wage-workers. All employers, self-employed workers, and unpaid family workers were excluded from the study. We also excluded 23,424 employees who did not have any health events. So 6,685 (the survey weighted sample size: 7,921) employees with ≥ 1 health event (the sum of SA and SP days) were included in the analysis of PP. Moreover, we excluded 692 employees who had missing values. Therefore, 5,993 (the survey weighted sample size: 7,274) employees were included for PP analysis.
Variables
Absenteeism, presenteeism, and PP
The number of SA days was calculated asking the following question: “How many sick leave days did you take in the past 12 months because of a health-related problem (or since starting your main paid job)?” The number of SP days was calculated asking the following question: “How many days did you go to work in the past 12 months despite an illness (or since starting your main paid job)?” The PP was calculated by dividing the number of SP days by the total number of health events (SA + SP days). This means that the value of PP ranged from 0 to 1.
Employment status
The employment status of the study participants was determined by period of contract. We theorized that employees with a contract term until retirement would have less job insecurities than employees with a fixed term. Moreover, employees with short-term contracts were expected to have more job insecurities than those with long-term contracts. Therefore, we classified the employment status into 3 categories by employment period: up to retirement age; of more than 1 year; and of less than 1 year. We defined stable workers as employees who had a contract period that lasted up to retirement. Unstable workers were wage-workers whose contract period was fixed and divided by the duration of their contracts into: unstable (≥ 1 year) and unstable (< 1 year). Also unstable workers with a contract period of more than 1 year are called "long-term workers,” whereas workers with a contract duration of less than 1 year are called “short-term workers.”
Covariates
Sociodemographic variables including age, gender, education, and occupational classification were determined from the questionnaire. Age was treated as a continuous variable. Education was classified into 3 categories: middle school graduate and lower, high school graduate, and college graduate and higher. Occupation was classified into 4 categories: professional, office, service & sales, and manual (blue collars & agriculture).
Work-related variables, namely the number of working hours per week, shift work, labor union, and company size were obtained from the questionnaire. The number of working hours per week was calculated by asking the following question: “How many hours do you work per week (excluding commuting and meal times)?” and was classified into 3 categories: 36–40 hours, 41–52 hours, and > 52 hours. Shift work was dichotomized as yes or no by asking the employees whether their job was shift-based. Similarly, labor union was dichotomized as yes or no by asking the employees whether they had a labor union. Company size was classified into 4 categories: < 5 employees, 5–49 employees, 50–299 employees, and ≥ 300 employees.
Furthermore, the variable “self-rated health status” was included because it influenced SP, and was determined by the question: “In general, how do you rate your health?” The answers ranged on a 5-point scale from “very poor” to “very good.” Employees who reported “very good” or “quite good” answers were considered as having good health, whereas those who reported “neither good nor bad,” “quite bad,” or “very bad” answers were considered as having poor health.
Statistical analysis
Logistic regression analysis was conducted to examine the association between employment status and PP, where PP was dichotomized as “≤ 0.5” and “> 0.5.” Employees with PP > 0.5 were more likely to attend work than to avail a sick leave when they had health events. In this analysis, we adjusted for covariates, including age, sex, education, company size, occupation position, working hours per week, shift work, labor union, and self-rated health. Pearson's χ2 test was used to assess the association between categorical variables, which were presented as frequencies and percentages. Continuous variables were compared using one-way analysis of variance or t-test and presented as mean ± standard deviations. The level of significance for all analyses was set at p > 0.05 with 2-sided testing. The survey weight was applied in all analyses. All statistical analyses were conducted using SPSS 23.0 (IBM Corp., Armonk, NY, USA).
RESULTS
We found that 6,685 (survey-weighted sample size: 7,921) of the 30,109 (survey-weighted sample size: 37,132) wage workers, accounting for 21.3% of the total sample, had experienced at least one health event within the 1 year preceding the survey (data not shown).
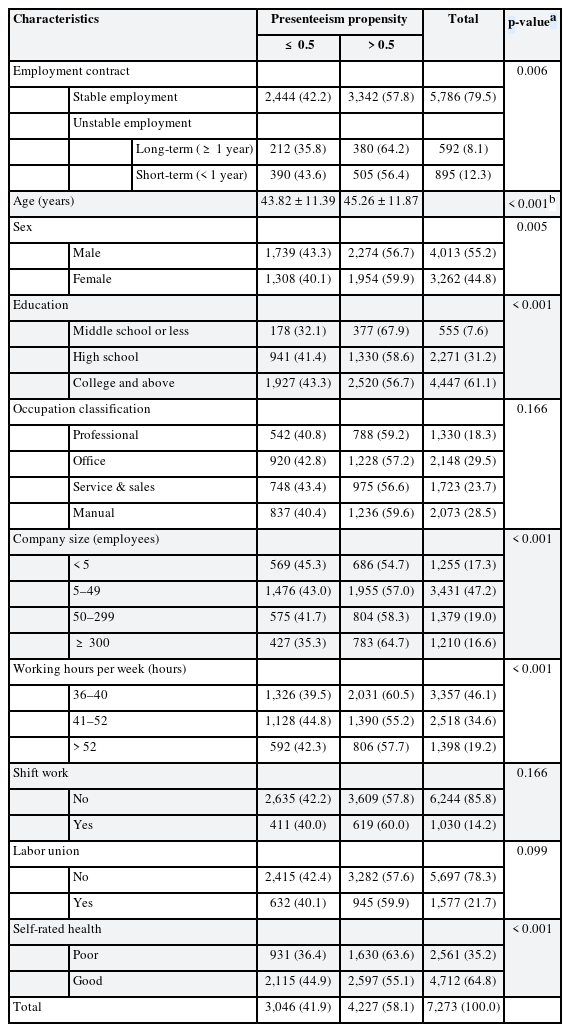
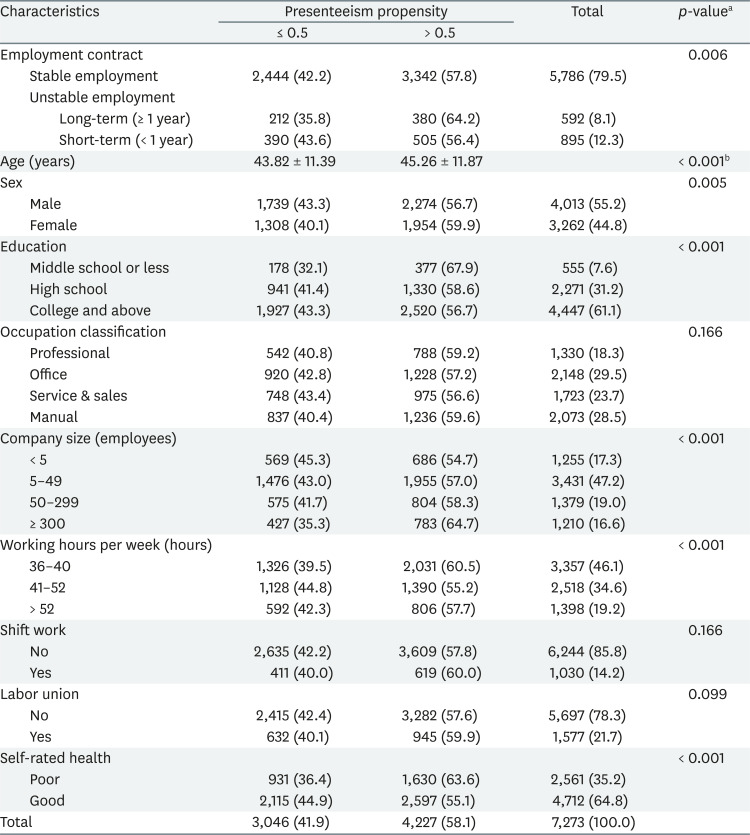
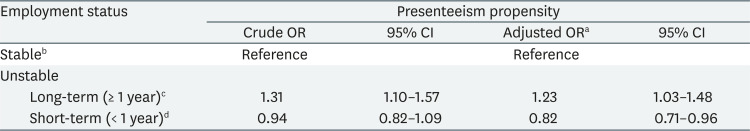
The general characteristics of participants are shown in Table 1. We analyzed a survey weighted sample of 7,274 employees. The average age was highest in short-term workers (< 1 year), followed by long-term (≥ 1 year) and stable workers. The proportions of employees who were male, obtained a college degree or higher, belonged to a labor union, and were in good health were found to be highest in the stable workers, followed by the long-term workers and the short-term workers. With regard to occupational positions, there was a higher proportion of manual workers among the short-term workers, whereas professional and office workers dominated the stable and long-term workers categories. All workers largely worked in companies with a size of 5–49 employees. The proportion of employees with > 52 working hours was 26.3% for short-term workers, higher than that for other workers (Table 1).
General characteristics of the study participants by employment status; findings from Korea Working Condition Survey, 2017
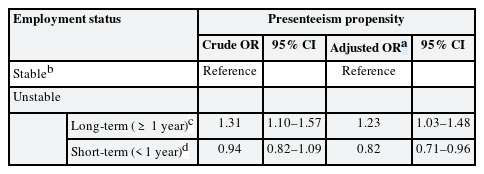
We used the Pearson's χ2 test to examine the differences in PP by general characteristics, and the results are presented in Table 2. Among all employees, 3,046 (41.9%) had PP ≤ 0.5, whereas 4,227 (58.1%) had PP > 0.5. The long-term workers were more likely to have a PP > 0.5 than the other workers. The mean age of the group with PP > 0.5 was 45.26 ± 11.87 years, which was higher than that of the group with PP ≤ 0.5 (43.82 ± 11.39 years). Moreover, the group with PP > 0.5 was more likely to have employees who were female, attained middle school or lower education, belonged to a labor union, worked for larger companies, and were in poor health. With regard to the number of working hours per week, the proportion of PP > 0.5 was highest among employees with 36–40 working hours per week (Table 2).
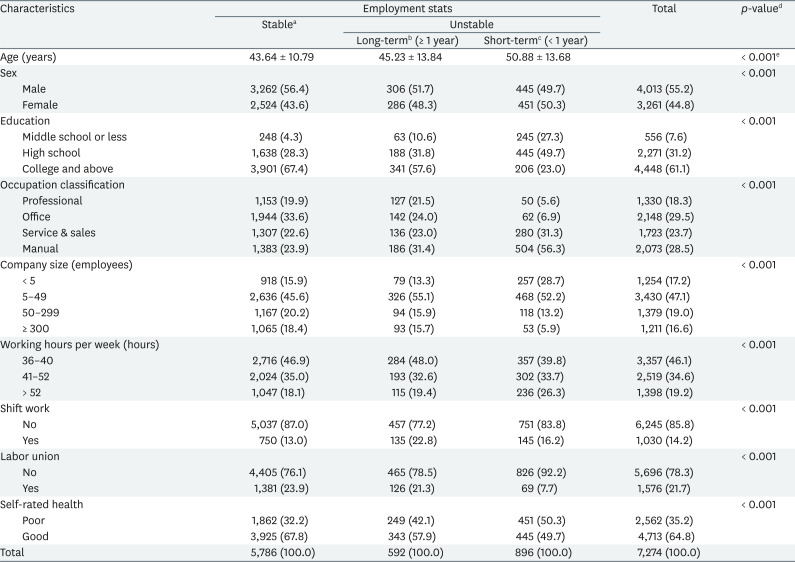
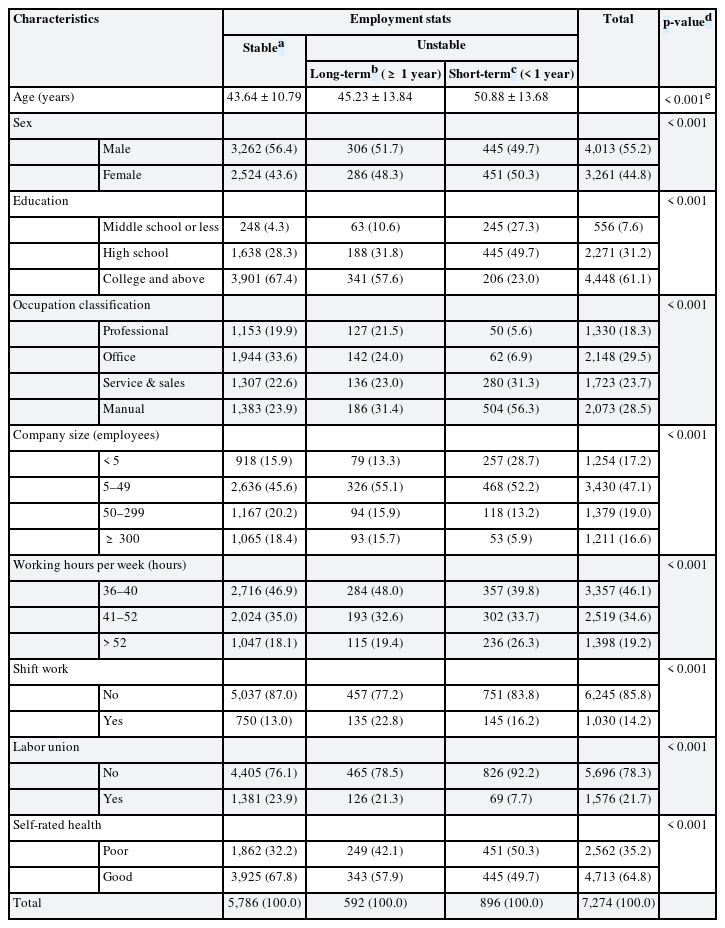
The association between employment status and PP was examined using the logistic regression analysis, and the results are summarized in Table 3. Compared with stable workers, long-term workers had higher odds of PP (odds ratio [OR]: 1.31, 95% confidence interval [CI]: 1.10–1.57), and short-term workers had lower odds of PP (OR: 0.94, 95% CI: 0.82–1.09); however, this difference was not significant. When we adjusted for covariates (i.e., age, sex, education, occupation classification, company size, number of working hours per week, shift work, labor union, and self-rated health), long-term workers showed a higher PP (OR; 1.23, 95% CI: 1.03–1.47), whereas short-term workers showed a lower PP (OR: 0.82, 95% CI: 0.71–0.96) (Table 3).
DISCUSSION
In this study, we found that 21.3% of Korean wage-workers had more than one health event in the year preceding the survey, and their mean PP was 0.59 (± 0.43); thus, on an average, they spent 59% of their days working when ill instead of taking a sick leave. This percentage was higher than the values reported in other studies that were conducted in Austria (59%), Canada (51.5%), and across 33 European countries (17%–61%) [282930]. The variation in PP might result from the use of different labor policies with regard to paid sick leave and differences in work attendance culture [30].
We found that long-term workers (≥ 1 year) and short-term workers (< 1 year) were more and less likely to have PP, respectively, than stable workers. We theorized that unstable workers would have higher job insecurity than stable workers whereas short-term workers would have higher job insecurity than long-term workers. The OR of PP was predicted to be the highest among short-term workers. However, the actual results differed from the initial hypothesis as the OR for PP was highest for the long-term workers, followed by stable and short-term workers.
The general characteristics of the groups with stable and long-term workers were different. The group of long-term workers had higher proportion of females, lower education rates, and higher rates of poor health than the group of stable workers. Female participants were more likely to be present at the workplace despite feeling ill due to gender social norms and stereotypes [31]. Low education level was related to poor health, and the association between poor health and SP has already been demonstrated in many studies [3233]. Moreover, long-term workers had greater job insecurity because they did not have permanent work contracts. Job insecurity was a strong predictor of SP because workers were under pressure to attend work despite being ill so as to maintain their jobs or increase their opportunities of becoming stable workers [14]. These differences seem to have caused long-term workers to have a higher PP than stable workers. Our results are similar to those of previous studies with regard to temporary workers who have contracts of ≥ 1 year [2030].
The OR for PP was lowest among short-term workers. Short-term workers had more unfavorable characteristics for health, which are associated with SP, than long-term or stable workers. These unfavorable characteristics were as follows: lower educational level, long working hours, and a high average age [263234]. Poor health can lead to both SP and SA and may have had a higher impact on SA in short-term workers [33].
One possible assumption is that the composition of short-term worker group was differed from that of long-term worker group. Although not shown in the table, the “daily” group who worked on a daily wage account for about 30.5% of short-term workers. Hence, the short-term workers had a very low chance of maintaining their jobs or becoming stable workers regardless of attending work when ill. Thus, they were less likely to be under any pressure to work when they were ill. Moreover, compared to stable workers, short-term workers might be less committed to fellowship and work ethics, which make one attend work even ill [3536]. In occupational classification, the short-term worker group showed a higher percentage of employees doing manual jobs and a lower percentage of employees with an education level of college or higher. In Korea, the rate of accidents is higher among blue-collar workers and those with lower education levels [37], and this result is consistent with the results of previous studies [3839]. In addition, compared with white-collar workers, blue-collar workers had more occupational injuries (e.g., musculoskeletal diseases or injuries), a higher number of poisoning accidents, and more days spent in hospital [40]; thus, short-term workers are more vulnerable to occupational injuries that force them to stay away from their workplace. Although not completely consistent with the results of this study, a similar OR for SP was observed between permanent and temporary workers (contracts < 1 year) in a previous study [20].
Similar to SA [1234], SP was associated with the poor health status of employees because it indicates the possibility of worker ill-health [1141]. Moreover, SP could contribute to the spread of communicable diseases, such as common cold or influenza, in the workplace, and eventually to the general population [42]. For example, on March 9, 2020, coronavirus disease cases were reported from a call center in Guro-gu [43]. This was one of the largest clusters of workplace infections in Korea. Unfavorable working conditions in call center and SP can contribute such large-group infections. It would have been possible to prevent community spread of the disease if workers with early symptoms stayed home. In addition, SP could hinder workers from receiving timely medical care, which could turn minor health conditions into more serious illnesses [44]. Furthermore, SP could delay recovery, resulting in increased costs. In terms of costs, the hidden loss of productivity due to SP accounted for 18%–61% of the total cost of workers' illness and was greater than the cost attributable to SA [45].
In Korea, unstable workers often face unfavorable working conditions. Discrimination against unstable workers exists in various forms, such as ease of dismissal or unfair wage payment [46]. With regard to paid sick leave, unlike other developed countries [47], Korea currently has no standard for paid sick leave in its labor law; paid sick leave is subject to the policies specific for individual companies. In workplaces without a paid sick leave system in place, employees have no choice but to avail a leave from their annual leave allowance when ill. After exhausting their annual leaves, employees with illnesses may have long unpaid absenteeism, which could lead to their retirement or dismissal. This means that unstable workers may be more prone to SP. In Korea, therefore, there is a greater need to focus on SP because of the sociocultural implications of job insecurity and lack of adequate provisions to avail paid sick leave.
The findings of this study suggest that long-term workers should be provided with leave allowance when they are ill. Entitlement to paid sick leave is influential in determining the rate of SP [48]. Korea has insufficient legal guarantees for paid sick leave and sickness benefit schemes when compared to other developed countries [49]. Therefore, policies such as increasing payment allowances for paid sick leave or expanding the health insurance coverage should be introduced to reduce the rate of SP [50]. In addition to losing their pay for the day, job insecurity compels unstable workers to attend work when they are ill [48]. Therefore, to ensure a sense of job security, the government should support unstable workers by converting their temporary positions into permanent roles. In addition, to improve the health status of their employees, organizations should implement workplace health promotion programs, such as safety and health education, which could eventually help decrease the prevalence of SP [51].
This study has several limitations that need to be addressed. First, the causal relationship between employment status and PP cannot be determined because of the nature of the cross-sectional study design. However, SP was less likely to be linked to unstable employment. Second, this study has not considered other possible confounding factors, such as income, job satisfaction, or other chronic diseases. Third, the estimation of SP and SA days was self-reported, which can be subject to recall bias.
CONCLUSIONS
This study used PP to identify employees' decision to work despite being ill, and found an association between unstable employment and SP. Because SP has negative health outcomes, the findings of our study imply that greater social efforts are required to reduce SP and enhance the health status of unstable workers.
ACKNOWLEDGEMENTS
The authors are appreciate for the Occupational Safety and Health Research Institute (OSHRI) and the KOSHA because of offering the raw data from the fifth Korean Working Condition Survey (KWCS).
Notes
Funding: This research is supported by Dong-a university research fund.
Competing interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Park JW, Cho SS.
Formal analysis: Park JW, Cho SS.
Methodology: Park JW, Cho SS.
Writing - original draft: Park JW.
Writing - review & editing: Park JW, Cho SS, Lee J, Hwang J, Kim JI, Kim BG, Hong YS.
Abbreviations
CI
confidence interval
KWCS
Korean Working Condition Survey
OR
odds ratio
PP
presenteeism propensity
SA
sickness absenteeism
SP
sickness presenteeism