Problems with diagnostic criteria for humidifier disinfectant lung injury (HDLI): two cases of radiologically improved HDLI
Article information
Abstract
Background
In Korea, to investigate the casual relationship between humidifier disinfectant and lung disease, four rounds of investigation and judgment were conducted. During this investigation, two adults who performed lung biopsy were recognized for their relevance between humidifier disinfectants and lung disease. At first, we did not think of the relationship to humidifier disinfectant because chest computed tomography (CT) finding of 2 cases were improved. However, they performed lung biopsy and it showed typical humidifier disinfectant lung injury (HDLI) pathologic findings, they could be recognized as HDLI. We report these cases here.
Case presentation
We selected 2 cases from the fourth-round investigation at Kangbuk Samsung Hospital. Patient of case 1 used humidifier disinfectants since September 2010. The patient was admitted 6 months later to the intensive care unit (ICU) due to severe dyspnea. Pathology following a lung biopsy revealed typical HDLI finding which was determined to be due to humidifier disinfectant exposure. Patient of case 2 used humidifier disinfectant from 2001 to 2008 for about 3 months each winter. The patient's cough and sputum production symptoms began in December of 2007. The patient was admitted to the respiratory medicine department due to worsening dyspnea. Pathology following a lung biopsy revealed typical HDLI finding. This was determined to have been caused by humidifier disinfectant exposure.
Conclusions
Because the typical radiologic findings associated with HDLI can improve over time, it is necessary to consider the revision of current diagnostic criteria that the presence of radiologic findings is important.
BACKGROUND
Humidifier disinfectant lung injury (HDLI) is caused by polyhexamethylene guanidine phosphate (PHMG) and oligo(2-(2-ethoxy)-ethoxyethyl)guanidinium-chloride (PGH) [12]. The pathologic finding most often associated with HDLI is pulmonary fibrosis involving the bronchioles and centrilobular lung parenchyma. Radiologically, HDLI is associated with diffuse centrilobular ground glass opacity (GGO) or nodules. These radiologic findings are known to often persist for more than 5 years after disease onset [34].
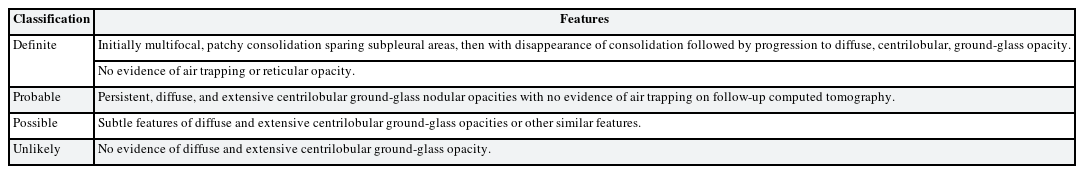
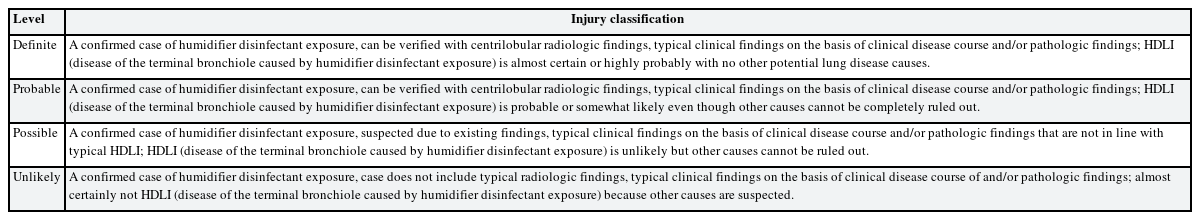
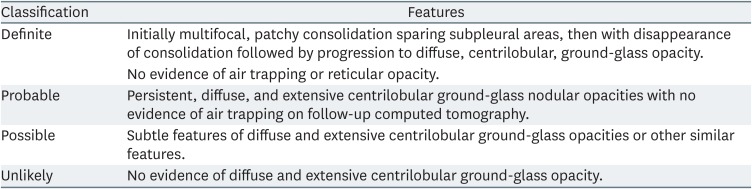
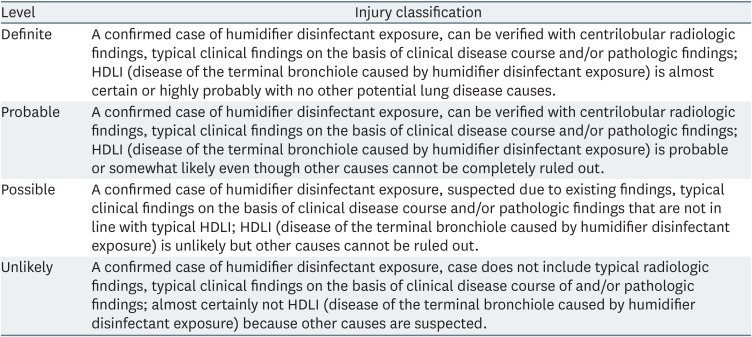
The diagnosis of HDLI is classified into four levels: definite, probable, possible, and unlikely. These classifications are based on pathologic, radiologic and clinical findings [35]. Detailed classification criteria are provided in Tables 1 and 2. Currently, a radiological trace is essentially required diagnosing the HDLI.
Six thousand six-hundred forty users of humidifier disinfectants have applied for compensation for damages, and in order to investigate the causal relationship between humidifier disinfectant exposure and lung disease, four rounds of investigation and judgment were conducted (1st: 361 people, 2nd: 169 people, 3rd: 752 people, 4th: 5,358 people). The investigation and judgment of HDLI has been completed in 5,616 out of 6,640 applicants, among these, only 8.6% (484 people) have been diagnosed with HDLI [7]. Kangbuk Samsung Hospital has been selected as one of 19 research institutes of fourth round and judged 206 people. Only 5 of them were recognized for their relevance to humidifier disinfectant. Three of them were children and only 2 adults who submitted past biopsy slides were recognized for their relevance between humidifier disinfectants and lung disease. At first, we did not think of the relationship to humidifier disinfectant because chest computed tomography (CT) findings of 2 cases were completely improved. However, they performed lung biopsy and it showed typical HDLI pathologic findings, they could be recognized as HDLI. At present, chest CTs are essentially required for the diagnosis of HDLI. If they did not have past biopsy slides and chest CTs, the association might not have been recognized. Therefore, we raise a concern about the current diagnostic criteria of HDLI by reporting two cases of improved findings on chest CT but with typical HDLI pathologic findings from past biopsy results.
CASE PRESENTATION
Methods
We selected 2 cases from the fourth-round investigation at Kangbuk Samsung Hospital. We reviewed medical records, laboratory findings, radiologic findings and pathologic findings of these 2 cases.
Case 1
Age/sex
34/Female
Chief complaints
Cough, dyspnea, weight loss.
Past history
None.
Medical history during the use of humidifier disinfectants
The patient's cough first presented in October of 2010. The patient received medical treatment for cough at a primary clinic in December of 2010, but experienced no improvements. Beginning in February of 2011, the patient experienced severe nighttime dyspnea and weight loss. In March of 2011, the patient visited the respiratory medicine department of first hospital and was admitted to the intensive care unit (ICU) due to suspected diffuse interstitial lung disease. The patient's vital signs at the time of hospital visit ware as follows: blood pressure of 120/80 mmHg, pulse rate of 105 beats/min, respiratory rate of 20/min, and a body temperature of 37.1°C. The patient was hospitalized from March 29, 2011 to April 9, 2011, and experienced symptom improvement following steroid therapy.
Laboratory findings
At the patient's first hospital visit, laboratory findings were as follows: white blood cell, 13,400 mm3 (86.0% segmented neutrophils, 1.3% eosinophils, 0.2% basophils, 8.2% lymphocytes, 4.3% monocytes); hemoglobin, 12.5 g/dL; platelets, 188,000mm3; blood urea nitrogen (BUN), 3.9 mg/dL; creatinine, 0.59 mg/dL; total protein, 6.7g/dL; albumin, 3.7 g/dL; aspartate aminotransferase, 18 IU/L; alanine aminotransferase, 14 IU/L; erythrocyte sedimentation rate, 4 mm/hr; and C-reactive protein, 0.53 mg/dL. An acid fast bacilli (AFB) smear was negative and there was no evidence of infection. The CD4/CD8 ratio of a bronchoalveolar lavage sample was 0.93.
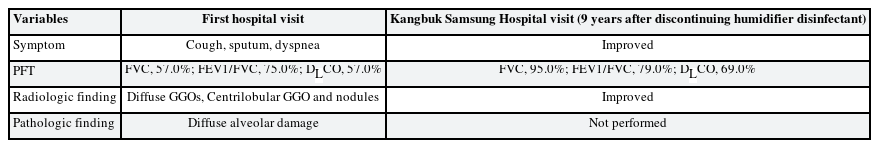
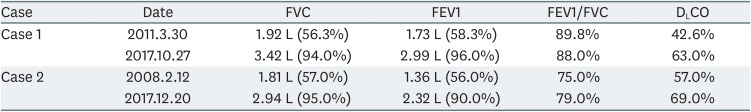
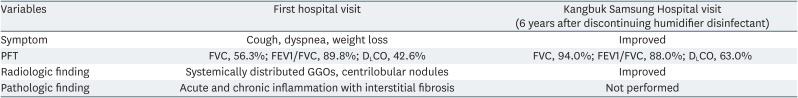
Pulmonary function test (PFT)
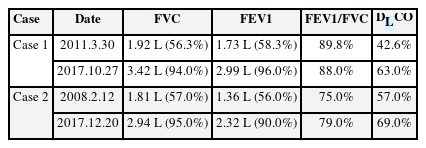
The patient's PFT results in 2011 were as follows (Table 3): forced vital capacity (FVC), 1.92 L (56.3%); forced expiratory volume in 1 second (FEV1), 1.73 L (58.3%); FEV1/FVC, 89.8%; and carbon monoxide diffusing capacity (DLCO), 42.6%. These results showed severe restrictive pattern.
Radiologic findings
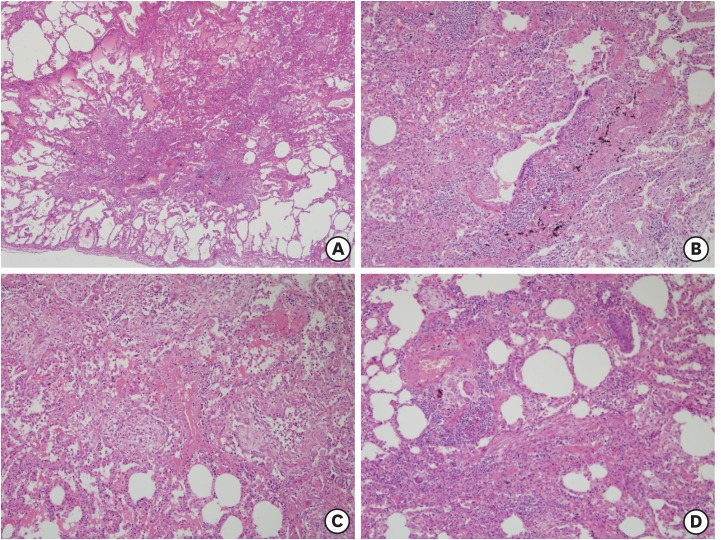
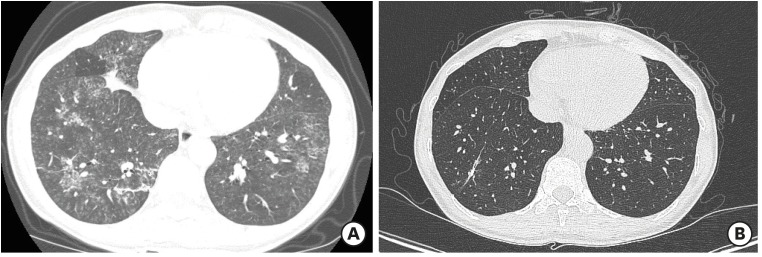
A chest high resolution computed tomography (HRCT) at the time of first visit hospital showed the appearance of acute diffuse interstitial lung disease, examples of which include acute eosinophilic pneumonia, hypersensitivity pneumonitis, diffuse alveolar damage, and interstitial pneumonia (Fig. 1A). Symmetrically distributed GGOs and small centrilobular nodules were observed. At the time, the relevance between humidifier disinfectants and lung disease was not clearly identified, so interstitial lung disease such as eosinophilic pneumonia and hypersensitivity pneumonitis were broadly suspected.
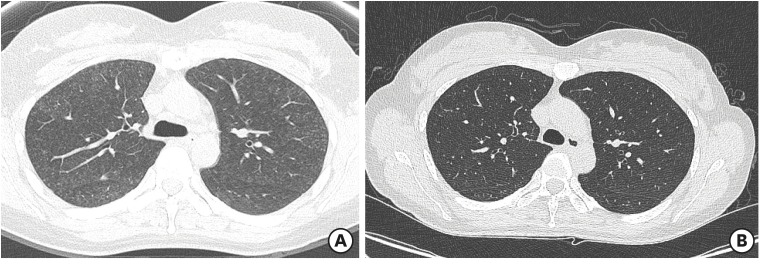
(A) Case 1 chest HRCT (at the time of first hospital visit): It shows the appearance of an acute diffuse interstitial lung disease such as acute eosinophilic pneumonia, hypersensitivity pneumonitis, diffuse alveolar damage, or interstitial pneumonia. Symmetrically distributed GGOs and small centrilobular nodules were observed. (B) A chest HRCT of case 1 (taken 6 years after discontinuing humidifier disinfectant at Kangbuk Samsung Hospital): Symmetrically distributed GGOs, small centrilobular nodules of both lungs at the initial CT were disappeared.
HRCT: high resolution computed tomography; GGO: ground glass opacity; CT: computed tomography.
Pathologic findings
A video-assisted thoracoscopic lung biopsy was performed on April 1, 2011. Acute and chronic inflammation with interstitial fibrosis, mainly along the peribronchiolar area were noted.
Humidifier disinfectant exposure history
The patient used humidifier disinfectants since September 2010. This patient's humidifier was located on the table right next to a bed. Thus, when the patient slept, steam from the humidifier was inhaled. A month after commencing with humidifier use, this patient began to cough. Humidifier disinfectants were not used after the patient's discharge in April of 2011. The patient was exposed to humidifier disinfectants for about 7 months, 8 hours a day.
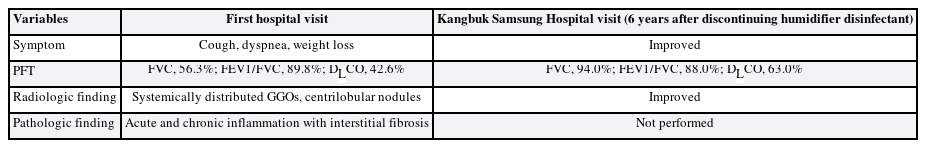
A review on the possibility of HDLI
This patient visited Kangbuk Samsung Hospital on October 27 of 2017 for an assessment of the humidifier disinfectant lung disease. PFT results at Kangbuk Samsung Hospital were as follows: FVC, 3.42 L (94.0%); FEV1, 2.99 L (96.0%); FEV1/FVC, 88.0%; and DLCO, 63.0%. Most indicators (FVC, FEV1) returned to normal compared to initial result except for relatively low DLCO (Table 3). A chest HRCT taken 6 years after discontinuing humidifier disinfectant use revealed that the symmetrically distributed GGOs and small centrilobular nodules in both lungs which were present upon initial CT imaging had disappeared (Fig. 1B). After reassessing pathology slides of 2011, we determined that humidifier disinfectant exposure was a definite cause of the patient's lung pathology. As a result, the patient's lung disease was definitively associated with humidifier disinfectant exposure. If biopsy slides did not exist, the disease would not have been recognized as HDLI. Because chest CT findings are important component in current diagnostic criteria and the patient's lung lesions were improved. Table 4 shows comparison of first hospital and Kangbuk Samsung Hospital visit of case 1 patient.
Case 2
Age/sex
42/Female
Chief complaints
Cough, sputum, dyspnea.
Past history
The patient was diagnosed with pulmonary tuberculosis in 2003 and was cured after 6 months of medication use.
Medical history during the use of humidifier disinfectants
The patient exhibited clinical signs including cough and excess sputum production starting in December of 2007. The patient experienced gradually worsening dyspnea, ultimately resulting in a first hospital visit and admission to the department of respiratory medicine (February 8 to 26, 2008). Initially, pneumonia or pulmonary tuberculosis was suspected, but there were no improvements with antibiotic use. The patient's symptoms improved with steroid treatment.
Laboratory findings
AFB staining was negative, and no pathogens were identified upon culture. Autoimmune disease markers were also negative.
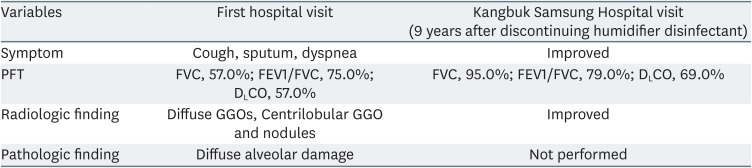
PFT
PFT results from 2008 were as follows (Table 3): FVC, 1.81 L (57.0%); FEV1, 1.36 L (56.0%); FEV1/FVC, 75.0%; and DLCO, 57.0%. These results showed a severe restrictive pattern.
Radiologic findings
An initial chest HRCT revealed diffuse ground glass opacity, centrilobular ground glass opacity, and nodules. Mild fibrosis in the right upper lobe and calcified nodules were also noted (Fig. 2A).
(A) Initial chest HRCT of case 2 (at the time of first hospital visit): It shows diffuse ground glass opacity, centrilobular ground glass opacity and nodules, and mild fibrosis in right upper lobe with calcified nodules. (B) Chest HRCT of case 2 (taken 9 years after discontinuing humidifier disinfectant use at Kangbuk Samsung Hospital): Centrilobular GGOs and peribronchial GGOs that were initially present in both lungs were disappeared. A postinfectious granuloma of RUL and diffuse air trapping in both lungs were observed.
HRCT: high resolution computed tomography; GGO: ground glass opacity; RUL: right upper lobe.
Pathologic findings
A lung wedge resection was performed on February 15, 2008. A bronchial obliterance organizing pneumonia pattern was identified in the resulting lung specimen (Fig. 3).
Humidifier disinfectant exposure history
This patient used a humidifier disinfectant every year from 2001 to 2008. The humidifier disinfectant was no longer used after moving. The patient was exposed to humidifier disinfectants for about 3 months each winter, 8 hours a day.
A review on the possibility of HDLI
In 2011, 3 years after discontinuing humidifier disinfectant use, a chest HRCT was performed at an outpatient clinic due to the patient developing bronchopneumonia. This HRCT revealed that the centrilobular GGOs and peribronchial GGOs present in both lungs in the initial HRCT had resolved. The patient visited the Kangbuk Samsung Hospital on December 20, 2017, nine years after discontinuing humidifier disinfectant use, for assessment of HDLI. The PFT results in 2017 were as follows: FVC, 2.94 L (95.0%); FEV1, 2.32 L (90.0%); FEV1/FVC, 79.0%; and DLCO, 69.0%. Most indicators (FVC, FEV1) returned to normal in 2017 compared to initial result except for relatively low DLCO (Table 3). A chest HRCT revealed that the centrilobular GGOs and peribronchial GGOs disappeared. Additionally, right upper lobe postinfectious granuloma and diffuse air trapping in both lungs were also observed (Fig. 2B). After re-reading the pathology slides of 2008, acute lung injury with a centrilobular pattern was observed and determined to probably be caused by the humidifier disinfectant exposure (Fig. 3). As a result, the patient's lung disease was determined to be associated with humidifier disinfectant exposure. Like the case 1, the disease would not have been recognized as HDLI without biopsy slides because the patient's lung lesions in chest CT were disappeared. Table 5 shows comparison of first hospital and Kangbuk Samsung Hospital visit of case 2 patient.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Kangbuk Samsung Hospital (IRB No. 2019-02-008). Written informed consent for publication of this case report was obtained from the patients.
DISCUSSION AND CONCLUSION
Since the humidifier disinfectant (PHMG and PGH) was found to be the cause of HDLI, the diagnostic criteria of HDLI were established - clinical, radiologic, pathologic criteria. Due to the strictness of the diagnostic criteria, most applicants were not recognized as victims.
In HDLI, pathologically, bronchiolar destruction and fibrosis are often accompanied by lung parenchyma inflammation. Radiologically, diffuse centrilobular ground-glass opacity and nodules are observed and often accompanied by a pneumothorax or pneumomediastinum [389].
Differential diagnosis for HDLI includes infection, hypersensitivity pneumonitis (HP), other interstitial lung diseases such as acute interstitial pneumonia (AIP), etc. Infection, however, result in a fever or positive pathogen cultures, neither of which occurred in the cases discussed above. Additionally, no cause for HP such as thermophilic actinomycete, fungus, animal or plant secretion exposure, or other, was identified. [10]. Furthermore, lung biopsy findings in both cases differed from those found in HP. In HP, inflammatory cells are predominant and non-necrotizing granulomas are characteristic. HDLI, on the other hand, is characterized by diffuse alveolar damage [8]. Chest CT findings in HDLI patients include focal patchy consolidation with subpleural sparing in the early phase and diffuse centrilobular nodules in the late phase; but, AIP is associated with diffuse bilateral infiltrates on CT images [8911].
The pathologic findings for the 2 cases discussed above served as the basis for diagnosing HDLI, however, radiologically-identified diffuse centrilobular nodules, a characteristic feature of HDLI, has not remained on HRCT images at present. Chest CT findings are very important component in current HDLI diagnostic criteria. If they did not have past biopsy slides and chest CTs, the association might not have been recognized.
Of the 206 patients assessed by our group previously, only seven patients (3.4%) had submitted biopsy slides in the 4-2th HDLI Survey conducted at Kangbuk Samsung Hospital. Furthermore, of these 206 patients, only 97 (47.1%) had submitted previous radiological images and 70 of them (34.0%) submitted previous chest CTs. At present, chest CTs are essentially required for the diagnosis of HDLI. Only seven patients submitted pathologic samples, and 66% of the patients had no previous chest CT images for HDLI judgment, so we could think cases that patients experienced HDLI in the past, but did not perform a biopsy at the time, and there are no special traces left in the current radiologic examination.
At present, the investigation and judgment of HDLI has been completed in 5,616 out of 6,640 applicants, among these, only 8.6% (484 people) have been diagnosed with HDLI [7]. Among applicants who were not recognized for their relevance to humidifier disinfectant, there is a possibility that there was a HDLI at that time, but the radiologic findings disappeared over time.
Final HDLI grades are determined based on the highest grade (definite, probable, possible, unlikely) of pathology, radiology, and clinical features [56]. These criteria were created in 2013 and do not reflect the problems mentioned above. The current criteria are the standard that describes the signs of a typical severe lung injury patient. At that time, this standard, aimed at identifying certain, clear HDLI patients, serves as the basis for excluding patients whose records were not complete or typical at the time.
In addition, a major error in the previous assessment process is that exposure assessment data were not taken into account in determining whether or not HDLI. At that time, exposure data were excluded from the judgment to enhance diagnosis and grading objectivity because HDLI was considered an unusual condition that was clearly distinct from other diseases. However, exposure assessment data should be considered together with radiologic and pathologic findings to determine HDLI because these radiologic and pathologic findings may change or resolve over time.
DLCO is an indicator of gas exchange in the lung [12]. Reduced DLCO may reflect damage of the peripheral region of the lungs. In the two cases discussed here, both patients' FVC and FEV1 recovered while DLCO remained low. In other words, in patients lacking previous data, reduced DLCO could be considered as one of diagnostic criteria.
We have raised a concern about current HDLI diagnostic criteria that chest CT findings are an essential component in judgement through two cases. Since chest CT findings can improve over time, it is not appropriate to determine the association between humidifier disinfectants and lung disease only with current chest CT results.
It is a limitation that we report only two cases from one hospital investigation. Therefore, it is necessary to analyze cases from other hospitals to see if there are more such cases. We recommend to reconsider the current diagnostic criteria of HDLI through detailed case review.
In conclusion, because the typical radiologic findings associated with HDLI can improve over time, it is necessary to consider the revision of current diagnostic criteria that the presence of radiologic findings is important. Also, long-term reduced DLCO can be considered as one of diagnostic criteria.
Notes
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Park SY.
Data curation: Nam MW.
Investigation: Nam MW, Park SY.
Validation: Suh BS, Ham SY, Son KH, Kim H, Kim HC.
Writing - original draft: Nam MW, Park SY.
Writing - review & editing: Nam MW, Park SY.
Abbreviations
AFB
acid fast bacilli
AIP
acute interstitial pneumonia
BUN
blood urea nitrogen
CT
computed tomography
DLCO
carbon monoxide diffusing capacity
FEV1
forced expiratory volume in 1 second
FVC
forced vital capacity
GGO
ground glass opacity
HDLI
humidifier disinfectant lung injury
HP
hypersensitivity pneumonitis
HRCT
high resolution computed tomography
ICU
intensive care unit
PFT
pulmonary function test
PGH
oligo(2-(2-ethoxy)-ethoxyethyl)guanidinium-chloride
PHMG
polyhexamethylene guanidine phosphate