A case of extensor pollicis longus (EPL) tendon rupture in an automotive assembly line worker: an ergonomic evaluation through job strain index (JSI) and musculoskeletal risk factor survey
Article information
Abstract
Background
We report a case of extensor pollicis longus (EPL) tendon rupture caused by repetitive motions and awkward posture on hand and wrist joints.
Case presentation
A 47-year-old right-handed man who worked for 15 years in an assembly line at an automotive manufacturing company has been diagnosed with a complete tear of right EPL tendon. We investigated the patient's occupational history in detail and evaluated the tasks ergonomically through musculoskeletal risk factors survey and job strain index (JSI) using the 22 task-related videos recorded by the patient. Three out of the 12 tasks (25%) were identified as high-risk work on the hand and wrist in the musculoskeletal risk factors survey in 2016. Among the 22 tasks analyzed by JSI, 11 tasks (50%) were evaluated as probably hazardous. In addition, he used localized vibration tools in 19 (86.4%) out of 22 tasks.
Conclusion
We concluded the patient's disease was probably caused by repetitive motion and improper posture of the hand and wrist, and the hand-arm vibration is a possible cause as well.
BACKGROUND
The extensor pollicis longus (EPL) originates from the posterior surface of ulna and interosseous membrane, and inserts to the base of distal phalanx of thumb [1]. EPL extends the distal phalanx of thumbs [2]. The rupture of EPL tendon can be caused by distal fracture of radius, distal incomplete dislocation of ulna, complication of steroids treatment and chronic inflammatory conditions such as tendon synovitis, rheumatoid arthritis of hand and wrist joints [345678].
There have been several case reports of EPL tendon rupture in chefs and tailors who repeatedly use their hands and wrists, and in athletes such as skiers, goalkeepers, kick boxers, and break dancers [910111213]. There were also case reports of a 30-year-old man who had played video games 8–10 hours per week for over 20 years, and a 29-year-old man who played a smartphone game all day long for 8 weeks [1415]. These previous cases only briefly reported patients' occupational and social history. The purpose of this study is to report a case of EPL tendon rupture in an automotive assembly line worker through detailed job analysis and ergonomic evaluation.
CASE PRESENTATION
Patient information
Forty-eight-year-old man.
Right handed.
Chief complaints
Pain and limited range of motion, thumb, right.
Present illness
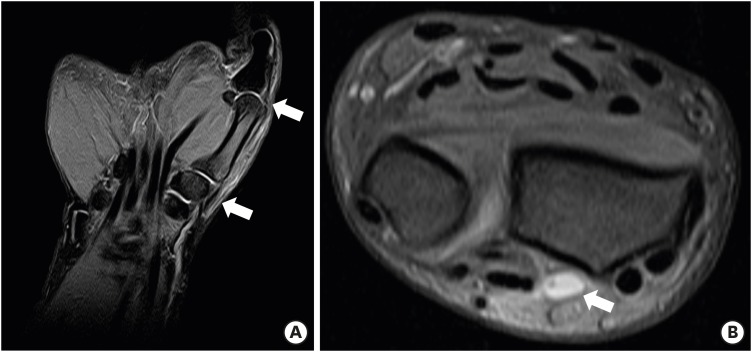
On November 6, 2014, while he was lifting a 3.1 kg antifreeze injection gun at the workplace, there was a crack sound and pain in the right wrist, and he could not move his right thumb. Before the onset of symptoms, there was no specific trauma or any other symptoms at the site. The ultrasonographic image taken on the day of the accident showed a complete EPL tendon rupture with a 4.31 cm gap in the right wrist (Fig. 1), and the magnetic resonance imaging (MRI) images taken 4 days after the accident also showed a complete tear of EPL tendon with a 5.6 cm gap in the right wrist (Fig. 2). The patient underwent immunohistochemistry including general blood tests to confirm the possibility of rupture by rheumatism. The C-reactive protein level was 0.16 mg/dL (normal range is less than 0.49 mg/dL), the rheumatoid factor level was 5.0 mg/dL (normal range is less than 20.0 mg/dL), the anti-cyclic citrullinated peptide antibody level was 7.0 U/mL (normal range is less than 17.0 U/mL) and the uric acid level was 8.4 mg/dL (normal range is from 3.5 to 7.0 mg/mL). He underwent a repair operation 4 days after the accident and he has recovered from the illness.
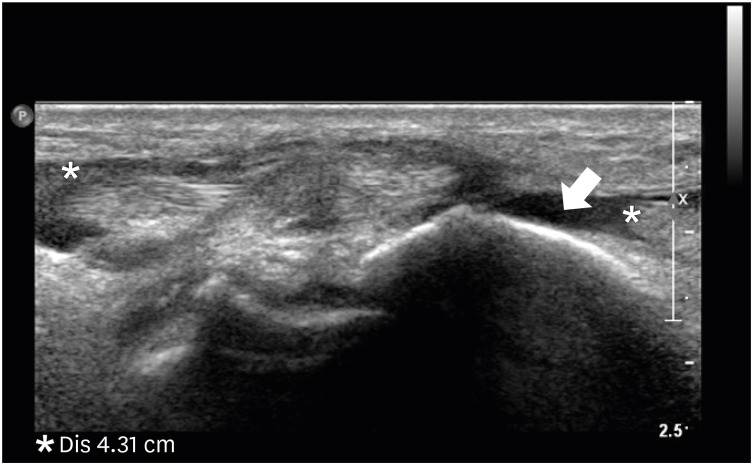
Ultrasonographic finding of the patient's right wrist. Extensor pollicis longus tendon rupture, wrist level, 4.31 cm gap. Hypoechoic fluid in the expected location of the tendon (arrow).
Past medical
He received medical treatment for lumbar disc herniation from 7th July 2001 to 26th February 2006 and he was allowed to claim worker's compensation insurance. He was treated conservatively for the right third trigger finger that occurred on March 27, 2008.
Social history & family history
He played badminton for about 15 minutes a day during lunch break in 2007, and he quit after the conservative treatment for his right third trigger finger. He was an ex-smoker (1.5 pack-years) and social drinker. There was no special family history.
Occupational history
He joined an automotive manufacturing company on February 13, 1995. He had engaged in assembly line work, shifting day and night for 10 hours a day, until February 2013, and he performed day shifting work for 8 hours a day from February 2013 to the present. After joining the company, he has worked for about 15 years in the same assembly line except for the period of medical care for his lumbar disc herniation. His job is the line work to assemble 36 cars per hour, he is not able to self-control the speed. His work groups consist of a total of four, with 1 group consisting of 12 people, and each group shifts monthly. According to the patient's statement, the labor intensity in the past was higher than that of the current work, and the difference in labor intensity from the different vehicle models was not significant. He did not wear any protective gear such as anti-vibration gloves during work.
Work-relevance evaluation
On January 16, 2017, he visited the occupational and environmental medicine outpatient clinic at a University Hospital in Busan, Korea for the work-relevance evaluation. First, the authors investigated the detailed job history by interviewing him. We performed a simple job simulation and confirmed that his tasks have repetitive motion and inadequate postures of the thumb and wrist. Especially applying pressure with extended thumb and hammering with extended wrist to deliver a strong and rapid impact seemed to be harmful. Fig. 3 shows his tasks considered burdensome. He complained that assembling door scarf, installing tailgate trim panel, and adjusting windshield glasses are particularly burdensome on his thumb and wrist.

Thumb and wrist joints burden of the patient's tasks. Extension of the thumb and ulnar deviation of the wrist are thought to be burden on the extensor pollicis longus tendon. (A, B) Extension of the thumb: applying pressure while installing door trim and trunk garnish (C) Ulnar deviation of the wrist: holding the hand-arm vibration tool while injecting antifreeze liquid (D) Repetitive motion of the wrist: tightening a screw with the wrench while installing air cleaner, battery cable, and duct.
We requested the results of musculoskeletal risk factors survey for the patient's workplace. In accordance with the Rule 657 of Korean Occupational Safety and Health Act, employers shall investigate the risk factors of the following items every 3 years when workers are carrying out musculoskeletal burden work [16].
A. Workplace situation: facilities, work process, work volume, work speed, etc.
B. Working conditions: working time, working posture, and working method.
C. Work-related musculoskeletal signs and symptoms.
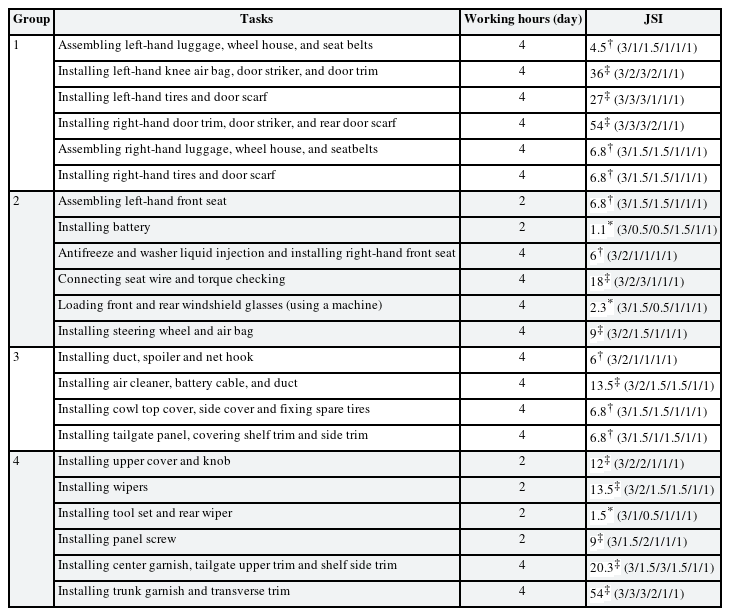
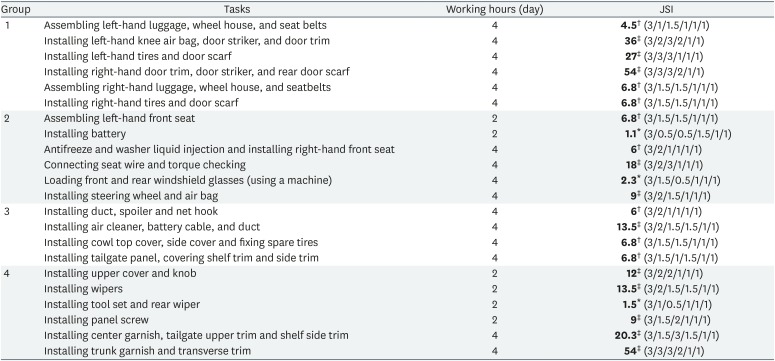
In the 2016 investigation, his work was divided into 12 tasks by the rule, and each task was divided into 6 burdened body parts (fingers/hands/wrists, arms/elbows, shoulders, neck, waist, and knees/legs). They were scored in terms of work posture, repeatability/static posture, strength and other burden work (hammering with hand or using vibration tools). Table 1 shows the results of 2016 musculoskeletal risk factors survey on fingers/hands/wrists. Adjusting position after mounting windshield glasses, tailgate weather strip fit, and installing tailgate trim panel were high scored tasks, and they have the similar tendency to the patient's subjective assessment of thumb and wrist burdens.
Results of 2016 musculoskeletal risk factors survey on fingers, hands, and wrists for the patient's work
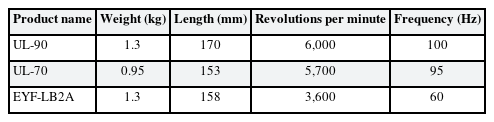
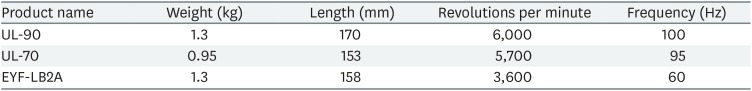
In order to evaluate the burden more quantitatively, we divided his work by 22 tasks focusing on the right thumb and wrist (job sampling) and requested him to record videos of the 22 tasks. We discussed the videos with him and retook several times, and finally obtained the total 22 task-related videos. We evaluated his work through job strain index (JSI) using these 22 task-related videos in order to analyze more objectively. JSI is an ergonomic evaluation method that mainly evaluates the upper extremities to quantitatively assess the ergonomic risk level of hand and wrist joints [1718]. Under the guidance of an ergonomic expert, authors analyzed the total 22 task-related videos focusing on his right thumb and wrist. The results of JSI analysis were tabulated in Table 2. Among the 22 tasks analyzed by JSI, 11 tasks (50%) were evaluated as probably hazardous.
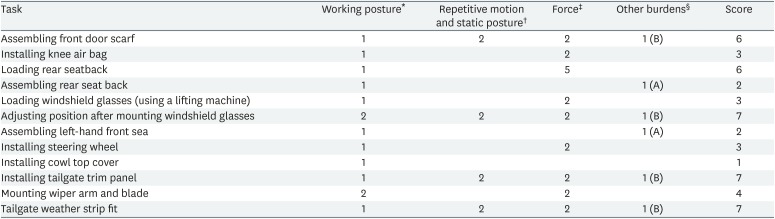
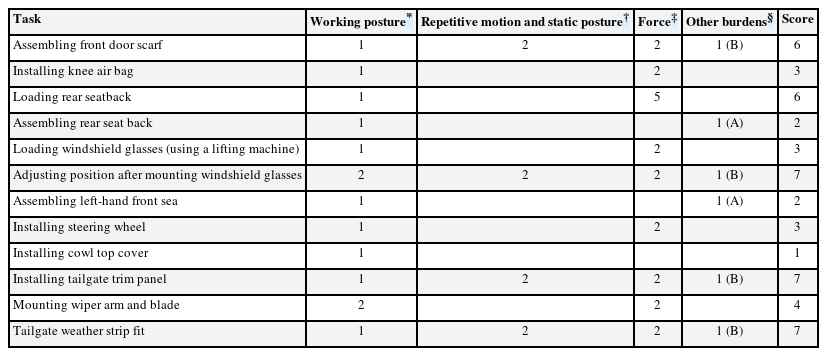
Additionally, most of the patient's tasks were using vibration tools. Among 12 tasks in the 2016 musculoskeletal risk factors survey, there were 2 tasks using a vibration tool for more than 2 hours and 4 tasks hammering with a hand more than 10 times per hour. In addition, there were 19 tasks using hand-arm vibration tools in the 22 task-related videos. Table 3 shows information of the vibration tools. The vibration acceleration of the tools could not be measured, so we could not calculate the cumulative vibration exposure. However, according to 2003 Korea Occupational Safety and Health Agency study, it is reported that about 16% of workers in the automobile manufacturing exceed 5m/s2 which is the exposure limit for European Union [19]. This case is also expected to be exposed to similar level. Considering his occupational history and the results of ergonomic evaluations, we determined that the EPL tendon rupture is highly correlated with the occupational exposure.
Ethics statement
Written informed consents were obtained from the patient for publication of this case report and any accompanying data.
DISCUSSION AND CONCLUSION
There are several major theories about the pathophysiological mechanism of EPL tendon rupture [41220]. The first theory is the rupture by hemodynamic factors. Since the area around Lister's tubercle is relatively narrow, it is easy to occur ischemia if the tendon sheath pressure increased [4]. Engkvist [20] performed micro-angiographic study and found that there was an avascular zone in the EPL tendon around Lister's tubercle that was nourished by diffusion from the synovial fluid. The second is the rupture by anatomical factors. Because EPL tendon turns sharply around the Lister's tubercle, it is vulnerable to increase pressure of the tendon sheath from trauma, fracture, and chronic inflammation, which may cause rupture of EPL tendon. The third is the inadequate biomechanical stress. Lloyd et al. [12] reported that in sports activities, improper hand and wrist posture cause excessive biomechanical force on EPL tendon so that degenerative changes occur by the tendon wear. In conclusion, EPL tendon rupture could be caused by the combination of hemodynamic, anatomical, and biomechanical factors.
The attritional rupture that generally occurs in the middle of the tendon is different from the high-energy rupture that occurs in the thinnest part of the tendon [15]. The EPL tendon rupture also occurred at the anatomical location near the Lister's tubercle which is the level corresponding to the attributional rupture. Particularly, considering the anatomical function of EPL tendons, extension of thumb and ulnar deviation which the patient usually take during work is probably harmful for the rupture. The orthopedic surgeon who performed the surgery also described that abrasion of the EPL tendon was observed in the surgical field and the disease is likely to be associated with the repetitive overuse of the hand and wrist. In addition, the patient used many hand-arm vibration tools while working. Hand-arm vibration can cause abnormalities in blood vessels, nerves, bones, joints and muscles, and cause localized blood flow disorders, which can lead to tendon wear [21]. The hand-arm vibration may also have affected some of the tendon rupture. However, there is a lack of research on the effects of local vibration on the tendon wear, so this needs to be supplemented by additional studies in the future.
The additional possible causes of the patient's illness can be considered. First, he developed a right third trigger finger in 2008, which may have affected the EPL tendon rupture. However, that accident was not a major injury such as a fracture, and the anatomical location of the disease is different. Second, his hobby was playing badminton. He played badminton for about 15 minutes a day in only 2007. Although it is known that EPL tendon rupture may occur in professional skiers, golfers and tennis players, it is unlikely that an ordinary person playing badminton for a short period of time as a hobby would have caused the disease. Lastly, the patient's blood test shows a slight increase in uric acid level but the other blood tests including C-reactive protein level were all with the normal ranges. Moreover, no abnormalities such as uric acid crystals (tophi) were found in the operation. Therefore, we assumed that the probability of rupture by gout is low. In conclusion, we determined the EPL tendon rupture was probably caused by repetitive motion and improper posture of the hand and wrist, and the hand-arm vibration is a possible cause as well.
In this study, we showed the general method of work-relevance evaluation conducted at an occupational and environmental medicine outpatient clinic. There is limitation in performing an ergonomic evaluation based on the task-related videos taken by the patient since the work place was not allowed to be visited due to the workplace regulation. However, we believe that this problem has been resolved through detailed job analysis and ergonomic evaluation.
We report that EPL tendons can be ruptured by improper posture and overuse of hand and wrist joints. The surveillance and follow-up management system should be established to prevent work-related musculoskeletal disorders (WMSDs). We also have to provide sufficient information about WMSDs and regular education for workers performing musculoskeletal burden work.
Notes
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Park S, Kim J.
Data curation: Park S.
Investigation: Park S.
Writing - original draft: Park S.
Writing - review & editing: Kim J.
Abbreviations
EPL
extensor pollicis longus
JSI
job strain index
MRI
magnetic resonance imaging
WMSD
work-related musculoskeletal disorder