The association between serum dehydroepiandrosterone sulfate (DHEAS) levels and job-related stress among female nurses
Article information
Abstract
Background
Dehydroepiandrosterone sulfate (DHEAS) is an endogenous steroid hormone produced by the adrenal gland. DHEAS has been suggested to play a protective role against psychosocial stress. The aim of this study was to investigate the association between job-related stress and blood concentrations of DHEAS according to occupational stress factors among female nurses.
Methods
A cross-sectional study was conducted among 118 premenopausal nurses from 4 departments (operating room, emergency room [ER], intensive care unit, and ward) of a university hospital. Participants were all rotating night shift workers who have worked for over a year and mean age of 33.5 ± 4.8 years. Data from structured questionnaires including the Korean Occupational Stress Score, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and Pittsburgh Sleep Quality Index (PSQI) were used.
Results
In the high job-related stressor group, scores of BDI, BAI, and PSQI were significantly higher than low-stressor group. ER nurses had relatively more work-burden related stressors, but they had significantly lower levels of anxiety and depression than other groups. And, ER nurses showed higher levels of DHEAS than the other department nurses. The differences were significant (p = 0.003). Additionally, there was a statistically significant difference even after adjusting for factors that could affect level of DHEAS, such as age, body mass index, drinking, and physical activity (p = 0.039).
Conclusions
This result suggests the possibility that DHEAS may play a role as a marker of proper stress management. The capacity to secrete DHEAS is not simply due to workload or job stressor but could be determined depending on how individuals and groups deal with and resolve stress. Proper resolution of stress may affect positive hormone secretion.
BACKGROUND
Dehydroepiandrosterone (DHEA) and cortisol are produced in different sections of the adrenal cortex; the zona fasciculata layer secretes cortisol while the zona reticularis layer secretes DHEA and its sulfated metabolite DHEA sulfate (DHEAS). DHEA and DHEAS are androgen precursors secreted in response to adrenocorticotropic hormone [1]. DHEA and DHEAS have been shown to have neuroprotective, antioxidative, anti-inflammatory, and antiglucocorticoid effects [2]. Previous studies showed that stress management, such as long-term exercise, increased DHEAS, which might have benefits in terms of improving an individual's health-related quality of life [34]. Considering this, DHEA and DHEAS have been suggested to play a protective role during acute stress as an antagonist to the effects of the stress hormone cortisol [5].
According to previous studies, different types of prolonged stress are suggested to negatively affect the function of the zona reticularis and thus inhibit the production of DHEA and DHEAS [67]. One source of prolonged stress is job stress at workplace [8]. Thus, DHEA has potential as an objective marker of job-related stress assessment. Level of job-related stress at work is determined by various factors including workload, working environment, reward, and individual aspects. In addition to these factors, the type and level of stressors may differ depending on the work department. The aim of this study was to investigate the association between job-related stressors and blood concentrations of serum DHEAS according to working conditions among female nurses.
METHODS
Study populations
One hundred eighteen female nurses (mean age, 33.5 ± 4.8 years) were recruited from a university hospital. All participants were rotating night-shift workers and those who have worked for over a year. We divided the participants into 4 departments: operating room (OR), emergency room (ER), intensive care unit (ICU), and ward. The numbers of participants were 29, 30, 30, and 29, respectively. Ages ranged from 25 to 49 years. Using self-reported structured questionnaire, we obtained information about age, history, drinking, smoking, exercise habits, health status including medical history and menopause, and tenure before blood collection. A drinker is defined as an individual who drinks more than 20 g of alcohol more than once a week. Exercise is defined as having regular exercise greater than 30 minutes per day more than twice a week. All participants were nonsmokers and premenopausal. Their body mass index (BMI) was calculated using the following formula: BMI = weight (kg)/height2 (m2). Exclusion criteria were as follows: taking medications, high blood pressure (systolic blood pressure above 140 mmHg or diastolic blood pressure above 90 mmHg), current infection, department move within 1 year or vacation within 2 months.
Blood sample collection and hormone analysis
After fasting for 8 hours, blood samples were drawn at the beginning of participants' workday (10:00 a.m.). Trained nurses collected the samples, which were transferred to the laboratory. The radioimmunoassay (RIA) method was used to determine DHEAS (DHEAS RIA CT; Asbach medical product, Obrigfeim, Germany) and cortisol (CORT-CT2 kit; Cisbio bioassays, Codolet, France) concentration in blood plasma according to the manufacturer's protocol. Detection limits were 1.2 µg/dL for DHEAS and 0.1 µg/dL for cortisol.
Job-related stress calculated by Korean Occupational Stress Scale (KOSS)
The KOSS was developed to measure occupational stress in the working population in Korea. KOSS is composed of the 8 subscales [9]. Cronbach's alpha used to evaluate the internal reliability of the subscale was 0.806. In addition, to compare subscales with similar characteristics, we divided the 7 subscales into 3 KOSS subtypes: 1) System related KOSS (inadequate social support, organizational system, lack of reward, and discomfort in the occupational climate), 2) Work-burden related KOSS (difficult physical environment, high job demand, and insufficient job control), and 3) Sub-total KOSS consists of 7 subscales excluding job insecurity. Because all the nurses worked in one hospital, job insecurity was excluded.
Beck Depression Inventory (BDI)
The BDI is a self-reporting questionnaire consisting of 21 questions addressing emotional, cognitive, synchronous, and physiological symptoms. Each item is scored from 0 to 3with a total score in the range of 0 to 63, and the Cronbach's alpha coefficient for internal consistency was found to range from 0.73 to 0.92 with a mean of 0.86 [10]. Scores of 0 to 9, 10 to 15, 16 to 23, and 24 to 63 are classified as indicating depression, mild, moderate, and severe depression, respectively [11].
Beck Anxiety Inventory (BAI)
The BAI is a self-reporting questionnaire consisting of 21 questions for measuring severity of clinical anxiety [12]. Each item is scored from 0 to 3 with a total score in the range of 0 to 63, and the Cronbach's alpha coefficient for internal consistency was found to range from 0.90 to 0.92 [1314]. Scores of 0 to 7, 8 to 15, 16 to 25, and 26 to 63 are classified as indicating no anxiety, mild, moderate, and severe anxiety, respectively.
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a self-reporting questionnaire that evaluates sleep quality over a one-month period consisting of 19 items with 7 components (subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction) [15]. Each component is scored from 0 to 3 with the total score in the range of 0 to 21, and the Cronbach's alpha coefficient for internal consistency was found to range from 0.80 to 0.83 [1617]. A participant is found to have a sleep disorder if the total score is higher than 5.
Statistical analysis
The general characteristics and psychosocial working conditions according to working department are provided in the form of descriptive statistics. Because DHEAS levels exhibited a right-skewed distribution, the data were subjected to a natural log transformation, its normality was verified, and statistical analysis was performed. ANOVA or χ2 test was utilized for the working department-dependent comparisons of general characteristics where appropriate. After the post-hoc test by Bonferroni method, differences between the groups were confirmed. The χ2 test, ANOVA, and Fisher's exact test were used to compare distributions of depression, anxiety, and sleep quality by working department. An analysis of blood concentrations of DHEAS and cortisol differences by working department was performed with ANCOVA after adjusting for the effect of age, BMI, drinking, and physical activity. The SPSS version 23.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Statistical significance was defined as p-value < 0.05.
Ethics statement
The study protocol was approved in advance by the Institutional Review Board (IRB) of Chonnam National University Hospital (IRB No. CNUHH-2018-185). In addition, each subject provided written, informed consent before participating.
RESULTS
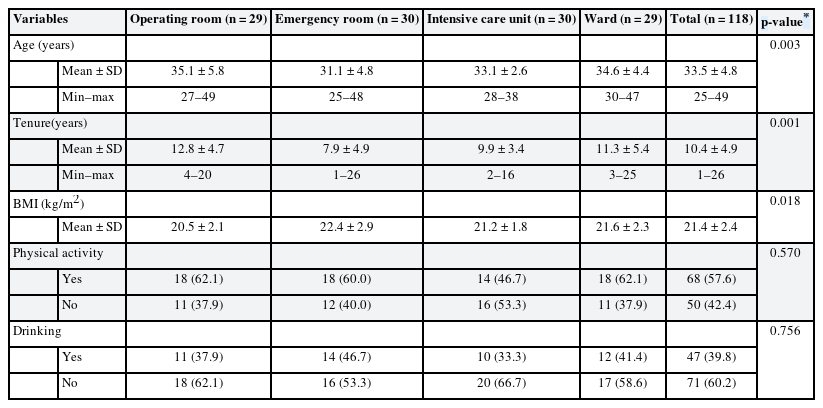
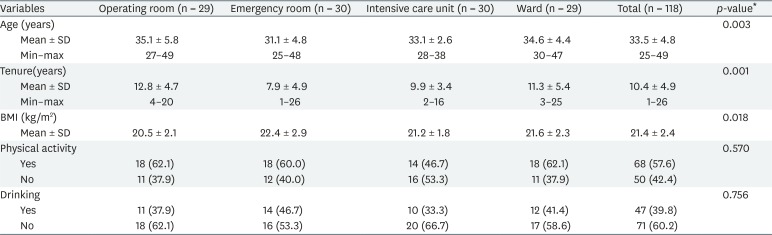
The mean age of participants was 33.5 ± 4.8 years. ER nurses' age and tenure were 31.1 ± 4.8 and 9.0 ± 4.9 years, respectively, significantly lower than those of the other departments. ER nurses' BMI was 22.4 ± 2.9 kg/m2 and significantly higher than that of the others. There was no significant difference between the departments in physical activity, drinking, and blood pressure (Table 1).
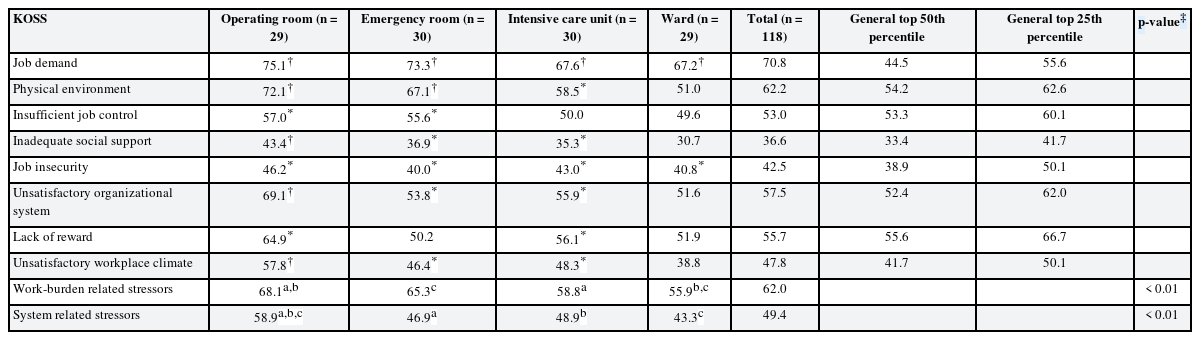
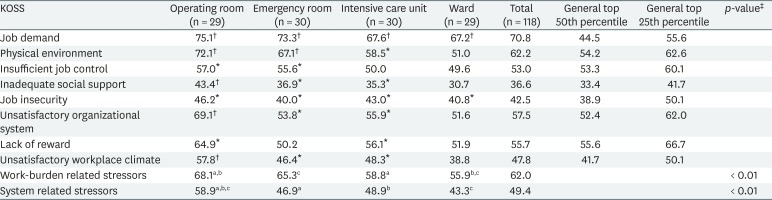
The KOSS was used to measure each department's job-related stressors. In 8 subscale scores, the participants were compared with the top 25th and 50th percentiles of Korean female workers [9]. A higher scale score means a higher stressor level. ER nurses were in the top 25th percentile of job stressors in job demands and physical environment. OR nurses were in the top 25th percentile of job stressors in job demand, physical environment, and unsatisfactory workplace climate. Ward nurses were in the top 25th percentile of job stressors in physical environment. ICU nurses had no job stressors in the top 25th percentile. OR nurses were in the 50th percentile in all job stressor items. ER nurses were in the top 50th percentile in all job stressor items except lack of reward. In comparison of the 2 KOSS subtypes performed to compare subscales with similar characteristics, work-burden related stressors were higher in OR and ER than in ICU and ward, and OR was significantly higher than ICU and ward, and ER were significantly higher than ward. System related stressors were significantly higher in OR than the other departments (Table 2).
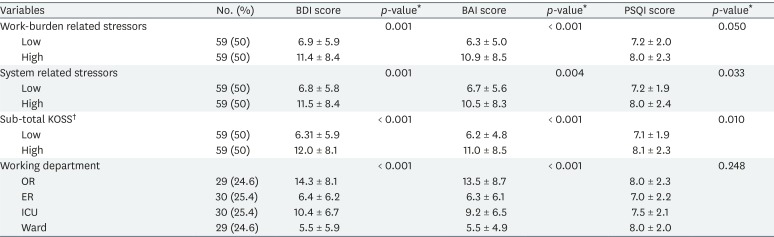
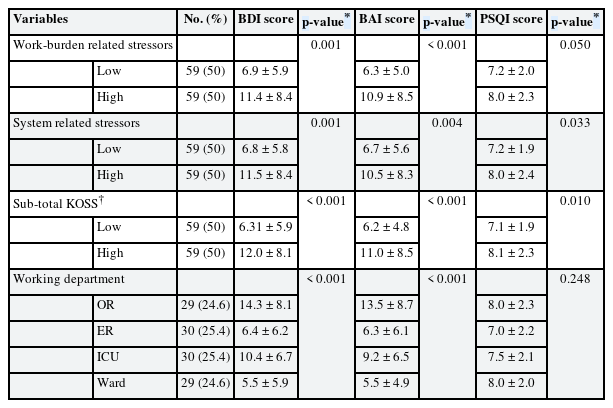
Mean scores of BDI, BAI, and PSQI were compared for 3 KOSS subtypes (work-burden related stressors, system related stressors, and sub-total KOSS) and each department. In the comparison of KOSS subtypes, BDI, BAI, and PSQI scores in the high-stressor group was significantly higher than low-stressor group. In the comparison of working department, OR and ICU nurses had higher BDI and BAI scores than ward and ER nurses, and this difference was statistically significant. There was no significant difference in the PSQI score between the departments. The percentage of those with severe depression and severe anxiety was higher in OR nurses, but this was not significant. While the participants were all rotating night-shift workers and their sleep quality was not good overall, there was no significant difference between the departments (Table 3).
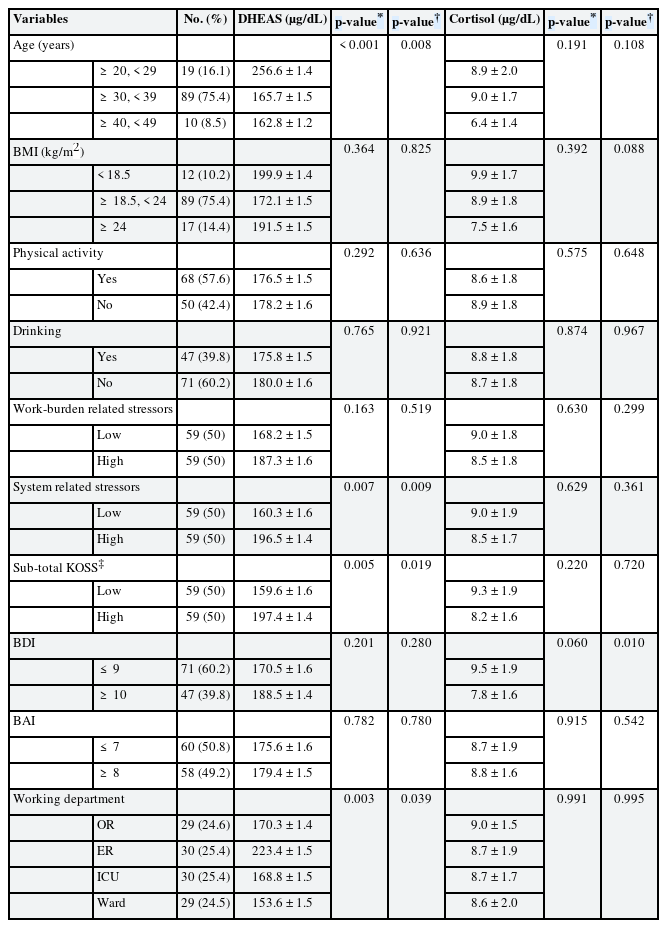
Distribution of depression, anxiety and sleep quality score according to KOSS subtype and the working departments in female nurses
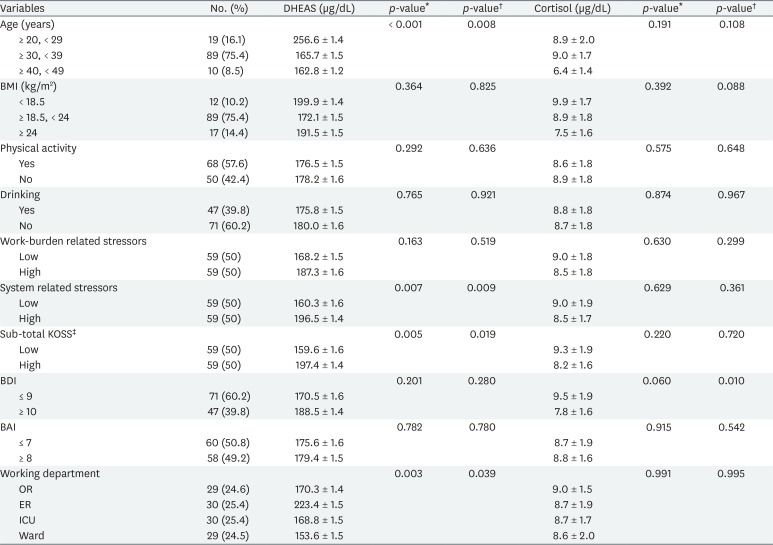
The mean serum level of DHEAS and cortisol was compared for 3 KOSS subtypes (work-burden related stressors, system related stressors, and sub-total KOSS). Three KOSS subtypes were divided into high and low stressor groups according to their scores. The mean serum level of DHEAS was significantly higher in high-stressor group of system related stressors and sub-total KOSS. After adjusting for confounders such as age, BMI, drinking, and physical activity, the mean serum levels of DHEAS were also significantly higher in the high-stressor group. There was no significant difference in the mean serum level of cortisol. The mean serum level of DHEAS and cortisol was compared depending on age group, BMI, physical activity, and working departments (OR, ER, ICU, and ward). The mean serum level of DHEAS showed significant differences in age and working departments. DHEAS was the highest in those in their 20s and negatively associated with age (r = −0.325, p = 0.001). In working departments, the mean serum level of DHEAS was the highest among ER nurses, and this was statistically significant. Such DHEAS differences between the departments were significant after adjusting only for age and still significant after adjusting for confounders such as age, BMI, drinking, and physical activity. There was no significant difference in the mean serum level of cortisol between the departments (Table 4).
DISCUSSION
In studies on effects of prolonged or chronic stress, it is preferable that DHEAS levels are measured rather than DHEA levels since they are more stable and show no or small diurnal variation. Concentrations of DHEAS are much higher (about 250–500 times) than those of DHEA, partly related to the fact that DHEAS has a longer half-life (7–9 hours) and lower clearance than DHEA. Perceived stress at work is associated with lower levels of DHEAS but not DHEA [18]. In a study looking at both DHEA and DHEAS in plasma, depressed patients had low DHEAS levels but normal DHEA levels [19]. Therefore, DHEAS is preferred over DHEA to compare the effects of prolonged stress at work.
DHEAS levels decreased in most studies when participants were under prolonged stress leading to exhaustion [6720]. DHEAS levels were negatively correlated with ratings of depressed mood. Specifically, higher DHEAS levels were associated with less depression, and this association was independent of age, physical activity, and weight change [21]. Increased DHEAS levels under conditions of stress may indicate a helpful process. In a study of 25 elite special operations soldiers exposed to prolonged and extreme training stress, soldiers experiencing fewer symptoms of dissociation and showing superior military performance had significantly higher ratios of plasma DHEAS to salivary cortisol [5]. Considering these results, DHEAS has been proposed to play a role in resilience and in successful adaptation to stress [5222324].
In this study, we examined differences in DHEAS levels by depression, anxiety, and job-related stressor according to working department in female nurses at a university hospital. In the high job-related stressor group, levels of DHEAS and scores of BDI, BAI, and PSQI were significantly higher than low stressor groups. As suggested by several studies, DHEAS levels increased in response to job-related stressors. Also, high job-related stressors are associated with depression, anxiety and low sleep quality. ER, OR, and ICU nurses had more job-related stressors than those in ward. However, the depression and anxiety levels were higher among OR and ICU nurses, and ER nurses were not. This can be summarized as follows: 1) OR nurses had more job-related stressors and higher depression and anxiety levels, 2) ER nurses had relatively more job-related stressors but lower depression and anxiety, 3) ICU nurses had relatively more job-related stressors but higher depression and anxiety levels, and 4) ward nurses had relatively fewer job-related stressors and lower depression and anxiety levels. OR, ICU, and ER nurses showed relatively high stress factors, so the OR and ICU nurses had higher BDI and BAI scores, but paradoxically, the ER nurses had lower BDI and BAI scores (Fig. 1). These findings demonstrate that nurses working in the same hospital could show significant differences in stress indices depending on the working department.
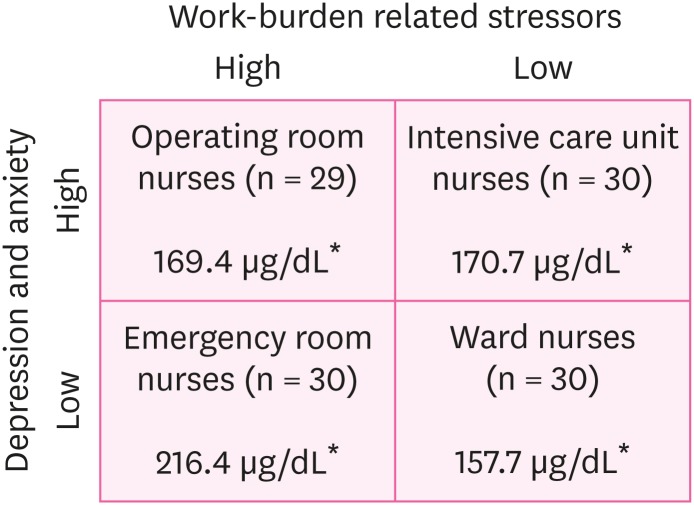
Distribution of work-burden related stressors, depression and anxiety according to the working departments in female nurses.
*Adjusted geometric mean of dehydroepiandrosterone sulfate, p-value = 0.039: calculated by ANCOVA adjusted for age, body mass index, drinking, and physical activity.
Considering the general physiological mechanism of DHEAS, while ward nurses with low levels of job-related stressors have a relatively low level of DHEAS, ER, OR, and ICU nurses with relatively high job-related stress levels should show increased DHEAS levels for acute stress and gradually decrease DHEAS levels if stress is sustained. In this study, we applied the maximum exclusion criteria to exclude sudden changes in the individual aspect, and all subjects were expected to show similar DHEAS levels. However, according to blood sampling result, ER nurses' DHEAS level was the highest among the 4 departments and statistically significant. Such a DHEAS difference was significant after adjusting for age, BMI, physical activity, and drinking. And the DHEAS levels of the remaining 3 departments were similar, with no statistically significant difference. These ER nurses' high DHEAS level could be the result of successful stress management. The following are a few possible reasons that could explain this.
First, there could be differences in not only the job-related stress level depending on the working department but also participants' systematic solutions to stress. Varying working environments and systems depending on the department affects how members control or address stress personally. For instance, even though a heavy workload is assigned, each individual can lower the level of stress as long as there is a structure in place that shares workload and responsibility appropriately at the department level or allows individuals to back one another up [25]. Furthermore, different stress management programs provided in each of the departments could affect members' stress levels. In fact, emergency workers are given 2 opportunities to participate in healing camps twice a year to help relieve stress and promote harmony among members of the department. In previous studies, DHEAS was used for stress-reducing interventions as a marker for the positive outcome [34], and the perceived stress level of those who showed a protective effect and participated in interventions decreased while their DHEAS level increased [26]. Also, stress management via long-term meditation or physical activity may prevent age-related decline in DHEAS production [2728].
Second, there is a financial reward. Except for wards, nurses working in OR, ER, and ICU receive additional monthly allowance. While OR and ICU nurses are receiving fixed allowance, ER nurse's allowance increase in proportion to the length of the service period and receive 5 times more than other departments if they work more than 3 years. Effort-reward imbalance (ERI) is well known to be associated with occupational stress. Cohort study of Juvani et al. [29] showed the combination of occupational stress and ERI had a higher hazard ratio (HR) for the pension of any cause, and especially when considering only the disability pension due to depression the HR of the combination of occupational strain and ERI increased. Likewise, in this study, ER nurses received more allowance than other department nurses and had the lowest lack of reward score in KOSS, suggesting that additional financial rewards had a positive effect on stress management.
Last, it could be attributable to differences in the fundamental nature of members (how to deal with crisis). ER workers are asked to perform rapid response and decision making relatively more often due to frequent emergency situations. In such an acute stress situation, they are frequently asked to enact a fight or flight response and must resolve problems as early as possible [30]. This response is recognized as “alarm,” the first step of general adaptation syndrome, and this goes through “resistance” and leads to the last stage of “recovery or exhaustion” [31]. Differences in the nature can affect how individuals adapt to such situations, and those workers who adapted themselves were repeatedly successful in their struggle and appropriate recovery in a situation where they were frequently required to choose between fight and flight, which would have had a positive effect on their hormones. Alternately, the individuals who were not able to overcome stress successfully in this process and had “exhaustion (or flight)” repeatedly got a job somewhere else or transferred to another department; as a result, there could be a healthy worker effect that only those members who adapted to such an environment remained. In other words, this result would have been found as the individuals who were innately more protective against stress and had better recovery endured better in a stressful situation, but it was not possible to determine which factors came first or later as this study used across-sectional design.
Additionally, further analysis of the KOSS subtypes showed that ER nurses had relatively higher work-burden related stressors and lower system related stressors when compared to ICU nurses. It is possible that the systematic intervention of ER nurses mentioned above affected the lower level of system related stressors than ICU nurses. One hypothesis is that the systematic interventions, individual nature and training process of ER department successfully lead ER nurses to overcome crisis situations (fight or flight) and adapt to stress. And stress management through these processes could have a positive impact on capacity to secrete DHEAS, just like long-term meditation or physical activity mentioned above. Of course, this study has not completely excluded the effects of age, personal aspects and health worker effect. In particular, DHEAS is strongly influenced by age, peaking at age 20 to 30, and then gradually decreasing, so the results should be interpreted with caution. This study was not able to perfectly stratify the age because of the limit of the selection of subjects. But considering the average age of the 4 departments was early 30s and it was significant even after adjusting for age, it is suggested that the characteristics of work departments (such as systematic interventions or how to work) may affect stress conditions and stress management.
In contrast to DHEAS level, there was no difference in cortisol level. According to a meta-analysis study of Hansen et al, in the 23 studies addressing association between cortisol in serum or urine and the psychosocial working environments, no consistent results were found [32]. Possible explanations for this are due to the distinct diurnal variation and the measurement situation (such as distress for blood sampling). Interestingly, the high depression group showed statistically significantly lower cortisol levels after adjusting for age, BMI, physical activity, and drinking. This could be the result of statistical coincidence or paradoxical hypocortisolism presented in some studies on post-traumatic stress disorder, chronic fatigue, chronic pain syndrome, fibromyalgia, and other functional somatic disorders [3334]. Although the mechanism has not yet been established, it is presumed that it may be related to individual vulnerability or early-life physical or sexual abuse [35]. Further research will be needed in the future.
This study has the following limitations. First, serum DHEAS levels are greatly affected by age; they are the highest in young adults and decline as age increases [36]. This study was conducted on small number of female nurses aged 25 to 49 and so is limited by the broad age range. After adjusting for age, this study's results still showed significant differences, but a future study should have a enough number of participants and perform a stratified analysis that reduces the age range of the participants. Second, another limitation is that the other factors that could have affected DHEAS levels (e.g., menstrual cycle, fertility, sexual information, private event, and stress management method) were not fully considered. In addition, blood was sampled only once to compare hormone levels. Nevertheless, to offset this weakness, blood sampling was performed on an empty stomach at 10:00 a.m. before day duty began. DHEAS has a slow metabolism and shows a low excretion rate in the kidneys, and its half-life is about 7–9 hours; as its diurnal variation range is relatively small, changes in concentrations are not large. Study of DHEAS level change in menstrual cycle of premenopausal women suggest that timing for DHEAS assessment is not important and that samples obtained at any stage of the menstrual cycle can provide a good indication of overall levels, as well as being reliable across different menstrual cycles [37]. In this study, there was no difference between groups in cortisol levels, which are known to have relatively large diurnal variations, and it is therefore reckoned that the study was performed such that the factors that would affect such hormones were controlled well. Third, the KOSS is a tool that assesses departments' stressors through comparison with median or quartile domain values, and it is difficult to quantify and compare it. While this study found that OR departments had relatively more stressors, this result does not directly indicate that OR departments' total stress was statistically significantly higher. However, in previous studies, it represented high validity by high correlation with the Job Content Questionnaire, Short Form of Psychosocial Wellbeing Index, and Mental Fatigue Scale [9]. Accordingly, it is reckoned that the KOSS could be used to identify the trends of the participants' job-related stress. Last, this study used a cross-sectional design, as mentioned earlier, and could not clearly state which factors believed to affect DHEAS levels came first or later. However, the above mentioned interventional methods, such as ER department's backup systems, participation in healing camps, and additional economic rewards, may have contributed to positive stress management.
This study has the following strengths. The participants had a high level of homogeneity as they were all female nurses in a single university hospital. While they worked in different departments, they were all rotating night-shift workers and had the same type of shift, number of working hours, and welfare system. In this study group with a high level of homogeneity, blood sampling was performed on an empty stomach for a set period (at 10:00 a.m. before day duty began) to rule out the effect of other confounders. In addition, the participants were all non-smokers, another factor affecting homogeneity.
In previous studies that used the KOSS to analyze job stressors, occupational stress was correlated with depression and anxiety in young women [3839] and strongly correlated with suicide ideation in subway workers [40]. This study found that there were significant differences in the serum DHEAS levels of female nurses across working departments. Such differences could not be explained simply by job-related stress levels. Although ER nurses were exposed to relatively more job-related stressors, their anxiety and depression levels were lower, and they showed a significantly higher DHEAS level, which is known to have a protective effect against stress. It is difficult to change the working environment with its individual members' effort or training. As long as an individual does not transfer to another department or workplace, he or she is exposed to the working environment for the long term, which affects health. Workers in working environments with a good system in place can effectively overcome a high level of stress. As such, the positive resolution of an appropriate level of stress would have had an effect on hormones such as DHEAS.
CONCLUSIONS
This result carefully suggests the possibility that DHEAS is likely to be a marker of proper stress management. The capacity to secrete DHEAS is not simply due to workload or job stress level but could be determined depending on systematic interventions, how individuals and groups deal with and resolve stress. Proper resolution of stress may have affected the positive hormone secretion. In the future, a cohort study involving more participants would need to be performed to derive findings after considering the important factors that could affect DHEAS such as age and what factors come first and later.
Acknowledgments
We thank all of the members of the Health Promotion Center at Chonnam National University Hwasun Hospital. We also thank the nurses for their participation.
Notes
Competing interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Cho S.
Data curation: Lim DY, Kang W.
Formal analysis: Cho S.
Investigation: Ahn JS, Lim HM.
Methodology: Park WJ.
Supervision: Park WJ, Moon JD.
Writing - original draft: Cho S.
Writing - review & editing: Park WJ, Moon JD.
Abbreviations
BMI
body mass index
BAI
Beck Anxiety Inventory
BDI
Beck Depression Inventory
DHEA
dehydroepiandrosterone
DHEAS
dehydroepiandrosterone sulfate
KOSS
Korean Occupational Stress Scale
Max
maximum
Min
minimum
PSQI
Pittsburgh Sleep Quality Index
IRB
Institutional Review Board
SD
standard deviation
ERI
effort-reward imbalance
RIA
radioimmunoassay
OR
operating room
ER
emergency room
ICU
intensive care unit
HR
hazard ratio